Antibiotics Across Generations: The Ripple Effect (Part 2/6)
Bacterial Inheritance: How Antibiotic Usage Today Shapes Our Children's Gut Microbiome Tomorrow
Welcome Back Gutsphere Friends,
As we continue our journey of understanding antibiotics and their far-reaching effects, we have now arrived at a particularly intriguing crossroad: the intersection of antibiotics and generations. This topic isn't just fascinating; it's also profoundly personal. Because when we talk about the inter-generational impact of antibiotics, we're not just discussing the implications for distant populations or future generations. We're talking about us, our children, and potentially our grandchildren.
Now, why is this an area that has piqued the interest of researchers and public health experts alike? Well, the seeds were sown by a 2020 study published in the journal Nature Communications[1]. The research suggested that if a pregnant mouse was given antibiotics, it could affect the gut microbiome of its pups. Not just that, but the change persisted until the third generation. It was a ground-breaking finding, demonstrating that antibiotic use could echo beyond the individual, rippling into future generations.
Then, there's the other aspect: Childhood antibiotic use. We've all been there. The first time our child has an ear infection, or a nasty cough, it's all too easy to seek the immediate relief that antibiotics promise. And there's no denying their benefits. Remember that ear infection? Without antibiotics, it could potentially lead to hearing loss. But the question we must grapple with is: At what cost do these immediate benefits come?
A study , estimated at least 30% of antibiotic prescriptions in ambulatory care settings in the United States from 2010 to 2011 were unnecessary[2].
Yes, the stakes are high, and the balancing act is delicate. But as we navigate this complex terrain together, we'll be guided by the beacon of evidence-based research and strive to bridge the knowledge gaps wherever they exist. So, let's dive in and delve deeper into the fascinating world of antibiotics across generations, understanding their impact, and seeking ways to mitigate any adverse effects while maximizing the benefits.
References:
A mother's microbiota: intergenerational transfer, https://www.nature.com/articles/nrgastro.2017.171
Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010-2011, https://jamanetwork.com/journals/jama/fullarticle/2518263
The Echoes of Antibiotics: An Insight into Their Inter-Generational Impact
The effects of antibiotics are not confined to the individual receiving the treatment. As we have seen, antibiotics can alter our gut microbiota, which has the potential for far-reaching implications. But this influence may not stop with us; there's a growing body of evidence suggesting that the impact of antibiotics might ripple through generations.
To understand the potential inter-generational effects of antibiotics, we first need to grasp how our microbiota can be 'inherited'. While our genetics are passed down from our parents through their DNA, we also inherit a living legacy from our mothers at birth: our initial microbiota. This microbial handover, primarily occurring during a vaginal birth, kickstarts the development of our gut microbiota, influenced later by our diet, lifestyle, and of course, exposure to antibiotics.
But what happens when this natural process is disrupted by antibiotics? Let's look at what the research tells us.
1. Antibiotics and early-life microbiota development:
An animal study found that mice treated with antibiotics early in life showed altered gut microbiota and immune responses. What was even more concerning was that these changes persisted into adulthood and were passed on to the next generation[1].
In humans, a population-based cohort study revealed that children exposed to antibiotics in utero had a significantly higher risk of developing infectious diseases in early childhood. These children had more hospital admissions for infections than those not exposed to antibiotics prenatally[2].
2. The Obesity Connection:
The relationship between the gut microbiota and obesity has been an area of active research. Studies have shown that antibiotics, by altering the gut microbiota, may contribute to weight gain. This risk could extend to the next generation.
In a study published in the International Journal of Obesity, researchers found that antibiotic exposure during pregnancy was associated with an increased risk of childhood overweight and obesity. This suggests a possible transgenerational effect of antibiotics on obesity risk[3].
3. Mental Health Implications:
Emerging evidence also indicates a link between alterations in the gut microbiota (dysbiosis) and neurodevelopmental disorders. Early-life antibiotic exposure could potentially disrupt the gut-brain axis, affecting neurodevelopment and contributing to disorders such as autism and depression. While still in the early stages, this research underscores the far-reaching implications of antibiotics[4].
We need to recognize that these findings, though significant, are the tip of the iceberg. There are still many knowledge gaps and unanswered questions. More research is needed to fully understand the inter-generational effects of antibiotics, including the mechanisms involved and the potential long-term implications.
What we can take away from this is a sense of responsibility. When we take antibiotics, we're not just influencing our health but potentially that of future generations as well. While antibiotics remain a vital tool in our medical arsenal, this understanding underscores the need for mindful use of these powerful drugs.
In our next section, we'll explore the delicate balancing act of prescribing antibiotics in childhood - when they are most often used, and when our microbiota are most vulnerable.
References:
Metabolic and metagenomic outcomes from early-life pulsed antibiotic treatment..https://www.nature.com/articles/ncomms8486
Antibiotics prescribed before, during and after pregnancy in the Netherlands: a drug utilization study. Pharmacoepidemiology and Drug Safety, https://pubmed.ncbi.nlm.nih.gov/23913654/
Prenatal exposure to antibiotics, cesarean section and risk of childhood obesity. International Journal of Obesity, https://pubmed.ncbi.nlm.nih.gov/25298276/
Altering the intestinal microbiota during a critical developmental window has lasting metabolic consequences. https://www.cell.com/fulltext/S0092-8674(14)00821-6
Effect of In-Utero Antibiotic Exposure on Childhood Outcomes: Methods and Baseline Data of the Fetal Antibiotic EXposure (FAX) Cohort Study, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6691671/
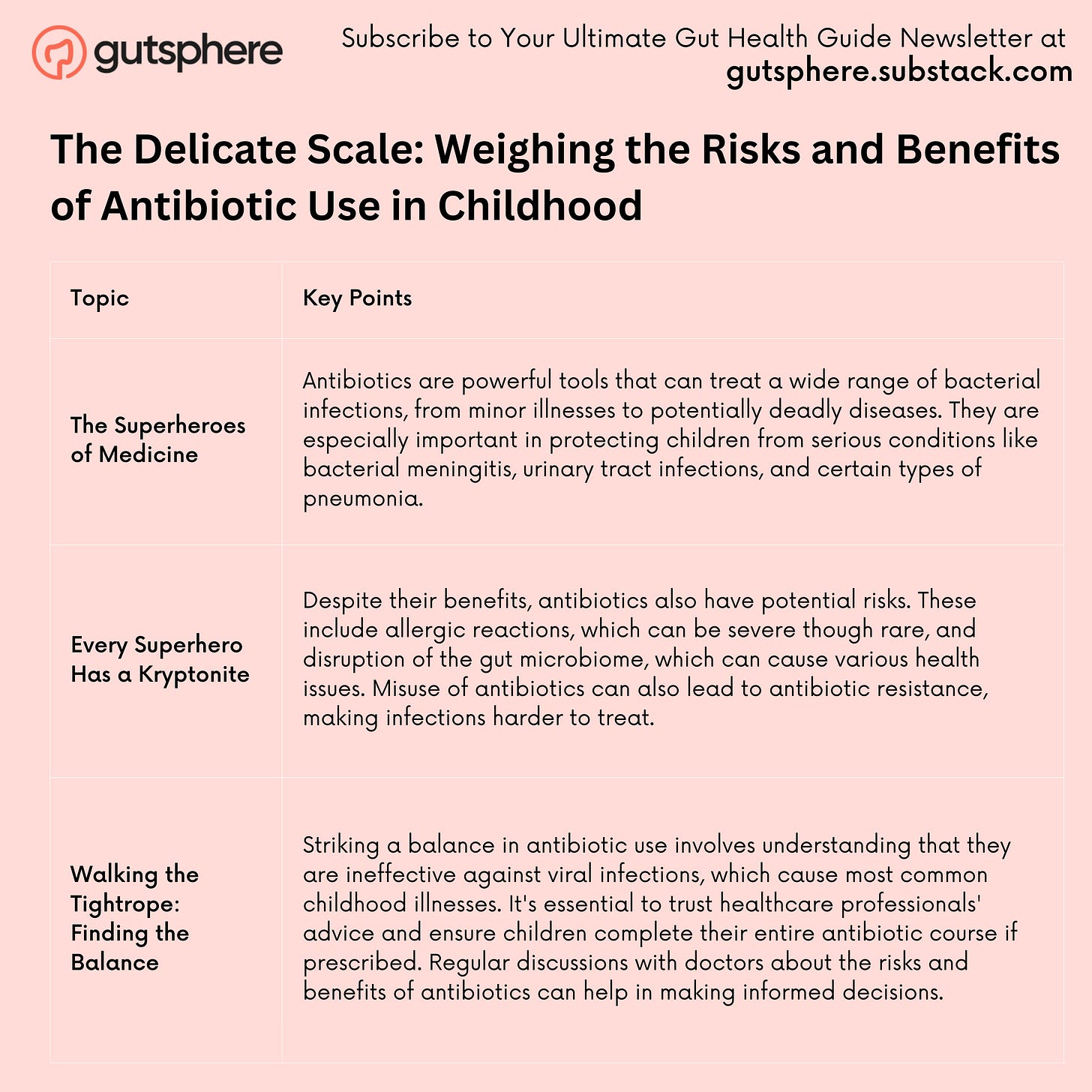
The Delicate Scale: Weighing the Risks and Benefits of Antibiotic Use in Childhood
Now, let's chat about something we've all come across, something that can get a bit sticky - the use of antibiotics for our kids. It's a little like stepping onto a tightrope. On one side, we have these incredible, lifesaving medicines that can kick even the toughest bacterial infections to the curb. But on the other side, there's a pile of potential problems that could emerge if we don't handle these powerful pills with the respect they deserve.
The Superheroes of Medicine
Let's start with the good stuff, the reason we're all grateful for antibiotics. Before these little gems were discovered, even a minor bacterial infection could be a death sentence. Fast forward to today, and we're able to fight off everything from a nasty bout of strep throat to a serious case of pneumonia. They're especially crucial for our kiddos, shielding them from dangerous infections like bacterial meningitis, urinary tract infections, whooping cough, and certain types of pneumonia[1].
And let's not forget the pre-emptive power of antibiotics! Before surgeries or dental procedures, they’re given to ward off any potential infections[2]. So, in many ways, antibiotics are like the superheroes of the medical world!
But Every Superhero Has a Kryptonite
Now for the not-so-fun part: the risks that come along with using antibiotics. First off, we've got allergic reactions. While most are just an itchy annoyance, severe reactions can occur. Anaphylaxis is rare, but it's definitely something we need to be on the lookout for[3].
Then there's the issue of our kids' gut microbiome. See, antibiotics are kind of like a bulldozer – they take down the bad bacteria, sure, but they also wipe out a lot of the good guys. This can lead to dysbiosis, a fancy word for an upset in the balance of the gut bacteria, which can result in everything from tummy troubles to immune and metabolic issues, and even impact brain development[4].
The real kicker, though? The emergence of antibiotic resistance, which is basically like giving bacteria a superpower. Overuse and misuse of antibiotics can create super-bacteria that laugh in the face of our once-effective treatments[5].
Walking the Tightrope: Finding the Balance
So how do we keep our balance on this tightrope? First things first, let's get one thing straight: antibiotics are not a magic bullet for all illnesses. They're absolutely useless against viral infections, which are behind most common childhood illnesses like colds, the flu, and many coughs and sore throats[6].
Avoid being that pushy parent who demands antibiotics when the doctor says it's a virus. They've got the training to make that call, and we need to trust their expertise.
If your child is prescribed antibiotics, make sure they finish the entire course. This is like making sure the superhero completes the mission, wiping out all the bad bacteria and leaving no survivors to form a resistance movement[7].
Lastly, don't be shy to have a conversation with the doctor about the benefits and risks of antibiotics. We're all on the same team here, working to keep our kids healthy while protecting the superpowers of antibiotics for future generations[8].
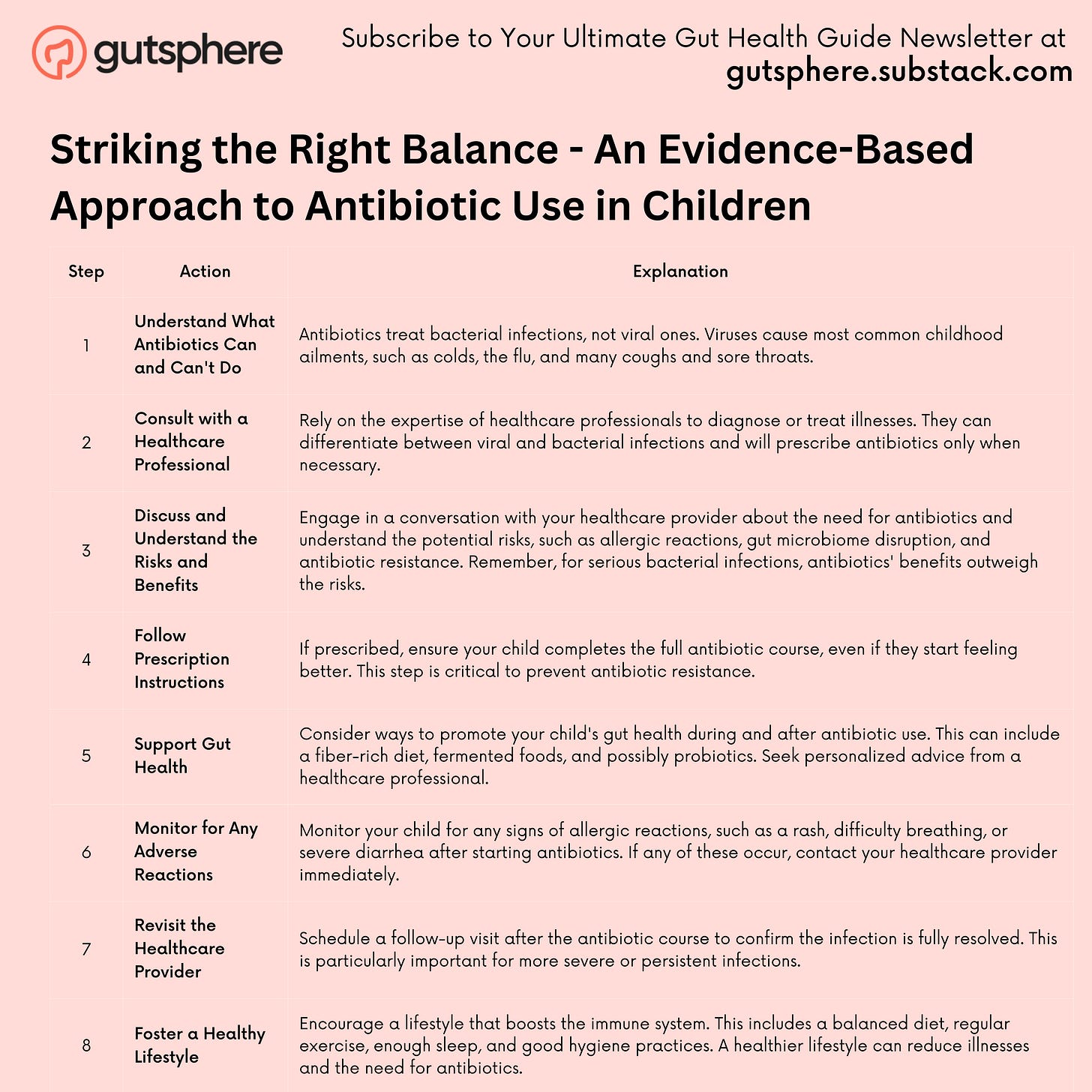
Striking the Right Balance - An Evidence-Based Approach to Antibiotic Use in Children
We understand the complexity and nuance involved in determining the right balance of antibiotic use for children.
Here is a step-by-step guide to help you navigate these crucial decisions:
Step 1: Understand What Antibiotics Can and Can't Do
Remember, antibiotics are designed to treat bacterial infections. They are not effective against viruses, which are responsible for the majority of common childhood ailments, such as colds, the flu, and many coughs and sore throats.
Step 2: Consult with a Healthcare Professional
Never attempt to diagnose or treat an illness without professional advice. Your child's pediatrician is an expert in distinguishing between viral and bacterial infections, and they will recommend antibiotics only when necessary.
Step 3: Discuss and Understand the Risks and Benefits
Open a dialogue with the healthcare provider about the necessity of antibiotics. Understand the potential risks associated with their use, including allergic reactions, disruption of the gut microbiome, and antibiotic resistance.
Keep in mind that for serious bacterial infections, the benefits of using antibiotics far outweigh the risks.
Step 4: Follow Prescription Instructions
If an antibiotic is prescribed, ensure your child completes the full course, even if they start to feel better before the medicine is finished. This is crucial in preventing antibiotic resistance.
Step 5: Support Gut Health
Consider ways to support your child's gut health during and after antibiotic use. This can include a diet rich in fiber and fermented foods, and possibly the use of probiotics. Consult with a healthcare professional for personalized advice.
Step 6: Monitor for Any Adverse Reactions
Keep a close eye on your child after they start an antibiotic regimen. If any signs of an allergic reaction occur, such as a rash, difficulty breathing, or severe diarrhea, contact your healthcare provider immediately.
Step 7: Revisit the Healthcare Provider
After completing the antibiotic course, consider a follow-up visit with the healthcare provider to confirm the infection is fully resolved. This is particularly important for more severe or persistent infections.
Step 8: Foster a Healthy Lifestyle
Encourage a lifestyle that promotes a strong immune system. This includes a balanced diet, regular exercise, adequate sleep, and good hygiene practices. A healthier lifestyle can reduce the frequency of illnesses and, by extension, the need for antibiotics.
Remember, every child is unique, and what works best for one might not work as well for another. Always seek personalized advice from a healthcare provider who knows your child's medical history and current health status. This guide should serve as a helpful tool to navigate these decisions, but it is not a substitute for professional medical advice.
Sources:
Nelson, E. Textbook of Pediatrics, 21st Edition. Elsevier, 2019., https://www.us.elsevierhealth.com/nelson-textbook-of-pediatrics-2-volume-set-9780323529501.html
Antibiotics: Misuse puts you and others at risk. Mayo Clinic, 2022. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/antibiotics/art-20045720
Anaphylaxis in Children. Johns Hopkins Medicine, 2022. https://www.hopkinsmedicine.org/health/conditions-and-diseases/anaphylaxis
Altering the Intestinal Microbiota during a Critical Developmental Window Has Lasting Metabolic Consequences, https://www.cell.com/fulltext/S0092-8674(14)00821-6
Antibiotic resistance. World Health Organization, 2021. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance
Viral Infections vs. Bacterial Infections: What’s the Difference? https://www.mayoclinic.org/diseases-conditions/infectious-diseases/expert-answers/infectious-disease/faq-20058098
Appropriate Antibiotic Use. Centers for Disease Control and Prevention, 2021. https://www.cdc.gov/antibiotic-use/index.html?
Antibiotics: Are you misusing them? Mayo Clinic, 2022. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/antibiotics/art-20045720
Conclusion
We've journeyed through the complex terrain of the antibiotics world, witnessing the tremendous benefits these drugs offer, especially in terms of treating life-threatening bacterial infections in children. However, we've also seen the dark side - from immediate risks like allergic reactions to the more profound implications of microbiome disruption and the threat of antibiotic resistance.
Perhaps most significantly, we've begun to unravel the deep-seated, inter-generational impacts of antibiotic use. The ripples of today's decisions could reach far into the future, affecting not just our children but their children too. It's clear that finding the balance is not just about the here and now, it's about safeguarding the health of generations yet to come.
As we conclude this part, remember: these potent pills are heroes, but even heroes need to be handled with wisdom and caution. Striking that delicate balance, under the guidance of healthcare professionals, is the best way to ensure these superheroes continue to save lives.
But the story doesn't end here. Just as we've seen that antibiotics can affect our children and future generations, we also need to understand their impacts at various life stages. How do antibiotics affect us differently as we grow older? And what are the potential links between antibiotic use and certain diseases? Could there be a hidden connection between antibiotics and the state of our mental health?
Next The Lifelong Impact: Antibiotics at Different Life Stages
In the next part of our journey, we'll explore these critical questions. We'll delve into the lifelong impact of antibiotics, and investigate the subtle yet significant ways they shape our lives at every age. From infancy to the golden years, we'll uncover the story of antibiotics - the story that's intimately intertwined with our own.
So, don't miss our next chapter, "The Lifelong Impact: Antibiotics at Different Life Stages." Let's continue this journey together and explore the compelling, yet complex narrative of antibiotics. Until then, stay curious, stay informed, and most importantly, stay healthy.
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
If you haven’t already subscribed then our sincere request, please subscribe.
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
GutSphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.