Colonoscopy Preparation Timeline Handbook. Episode 9 T-6 HOURS
No liquid + Reminder for Driver
Introduction
Good morning, and welcome back to the final stretch of our Colonoscopy Preparation Podcast series. With just a few hours left until your procedure, it’s crucial that we go over the last-minute details to ensure you’re fully prepared. I’m Bimal Maharjan, and I’m here to guide you through these last important steps.
Source of Information:
Our tips this early morning are grounded in trusted gastroenterology practices, designed to ease your preparation and reduce anxiety as you approach the procedure time.
Recap of Previous Episodes:
In our last episode, T-1 Evening, we discussed how to manage your final prep solution intake, ensure proper hydration, and set up a comfortable environment for a restful night. Now, as you awaken, we’ll address any overnight changes and prepare you for the day ahead.
Connection and Series Overview:
As this series comes to a close, each episode has been a step in your journey to a successful colonoscopy. Today’s episode is the culmination of all your preparation efforts.
Episode Overview:
This morning, we will cover how to handle any remaining prep steps, finalize your preparations for traveling to the clinic, and discuss strategies to manage any last-minute anxiety.
Stay with us, and you will enter the clinic prepared, calm, and ready. These last hours are key, and we’re here to ensure you handle them with confidence.
No Liquid Consumption
Clarification on Restrictions:
Q1: Can you define 'no liquids'? Does this include water, clear broths, or medications?
Until what exact time am I allowed to consume clear liquids, and when must I strictly start the 'no liquid' period?
Clarification on Restrictions:
Understanding when to stop consuming liquids, including water, is vital for a safe and effective colonoscopy. Let's define what 'no liquids' really means and discuss the specific cutoff time for drinking them.
Definition of 'No Liquids':
Guideline: 'No liquids' means abstaining from all forms of liquids, including water, clear broths, tea, and any other beverages.
Evidence: This practice is essential to ensure an empty stomach, which reduces the risk of complications such as aspiration during anesthesia.
Timing for Last Liquid Consumption:
Guideline: The cutoff time for consuming any liquids is typically 2 to 4 hours before your scheduled arrival at the clinic. This period allows your stomach to empty sufficiently.
Example: If your procedure is at 8 AM, and you're told to arrive at 6 AM, your last intake of clear liquids should be no later than 2 AM.
By adhering to these guidelines, you help ensure a smooth procedure with minimal risk of complications. Always follow the specific instructions provided by your healthcare team, as timing may vary based on your individual health needs and the specifics of your procedure.
Medication Intake:
Q2: How should I take any essential medications during the 'no liquids' timeframe? Are there exceptions to the 'no liquids' rule for critical medications, and how should I manage them?
Medication Intake:
Taking essential medications during the 'no liquids' timeframe can be challenging, but it's important to manage them correctly to maintain your health and safety.
Taking Essential Medications:
Guideline: Essential medications may be taken with a small sip of water during the 'no liquids' period, under the guidance of your healthcare provider.
Evidence: A minimal amount of water used to take necessary medications is generally considered safe and does not interfere with the requirement for an empty stomach.
Exceptions for Critical Medications:
Guideline: Certain critical medications, such as heart or blood pressure pills, may need to be taken the morning of the procedure. Discuss these exceptions with your doctor.
Example: Your healthcare provider may instruct you to take your blood pressure medication with just enough water to swallow the pill safely.
Carefully managing your medication intake during the 'no liquids' period is crucial. Always consult with your healthcare provider about which medications are essential and how they should be taken on the day of your colonoscopy. Following these guidelines helps ensure your safety and the success of your procedure.
Reminder for Driver
Transportation Coordination:
Q3: What information does my driver need to know about pick-up times and locations post-procedure? How long is the colonoscopy expected to last, and how much time should my driver plan to wait?
Driver's Role and Requirements:
Q4: Does the person picking me up need to come inside the facility, or can they wait in the car? What if my designated driver cancels at the last minute? What are my options?"
Transportation Coordination:
Coordinating with your driver is key to a stress-free experience post-procedure. Let’s go over what your driver needs to know about pick-up times, locations, and their role during this process.
Information for Driver:
Guideline: Inform your driver of the exact location and time of your procedure, and provide them with the expected duration and pick-up time.
Example: Colonoscopies typically last 30 to 60 minutes, with recovery time varying from 30 minutes to an hour. Ensure your driver knows to be available to pick you up approximately 2 hours after the procedure starts.
Driver’s Role and Requirements:
Guideline: Drivers should check in at the facility reception upon arrival to confirm their presence and availability to take you home.
Example: Some facilities may allow drivers to wait in the car, but they should be ready to come inside if called upon.
Contingency Plans:
Guideline: Have a backup plan in case your primary driver cancels. Know the contact numbers of reliable taxi services or ask the facility if they offer transportation services.
Example: Keep a list of alternative contacts or transportation apps ready on your phone as a precaution.
Ensuring your transportation details are clear and having a backup plan in place are essential steps to a smooth transition home after your colonoscopy.
Health and Safety Concerns
Addressing Hunger and Weakness:
Q5: What should I do if I feel extremely weak or dizzy due to not consuming any liquids? Are there signs of dehydration I should be vigilant about during the 'no liquids' period?
As you adhere to the 'no liquids' rule before your colonoscopy, it's important to be aware of how to manage any signs of discomfort or dehydration.
Managing Hunger and Weakness:
Guideline: Feeling weak or dizzy can occur; sit or lie down to minimize the risk of falls. Communicate any severe symptoms to the medical staff immediately.
Example: If you feel overly weak or dizzy, alert a nurse or doctor at the facility. They can assess your condition and provide necessary interventions.
Signs of Dehydration:
Guideline: Be vigilant about symptoms such as excessive thirst, dry mouth, very dark urine, or a significant decrease in urination.
Example: Monitor yourself for these signs, and report them to healthcare staff as they could necessitate medical attention to prevent further complications.
Taking care of your health by recognizing signs of weakness and dehydration, and knowing how to respond, is crucial during the 'no liquids' period. Your well-being is the priority, and taking these precautions ensures your safety.
Remember, following these guidelines will help you manage the logistics of transportation and maintain your health during the preparation for your colonoscopy. These steps are designed to support a successful and safe procedure.
Emergency Contacts:
Q6: Whom should I contact if I experience severe discomfort or symptoms during the 'no liquids' period?
Emergency Contacts:
As you enter the 'no liquids' period, knowing whom to contact in case of severe discomfort or symptoms is crucial for your safety.
Guideline: Have the contact information of your gastroenterologist or the medical facility where your colonoscopy will be performed readily accessible.
Example: Program these numbers into your phone and also have a physical copy handy, perhaps attached to your refrigerator or in your wallet.
Being prepared with the right contact information allows you to quickly address any urgent issues that arise, ensuring your well-being is maintained throughout the preparation process.
Pre-Procedure Anxiety
Managing Anxiety:
Q7: How can I manage anxiety or nervousness in the final hours leading up to the colonoscopy? Are there relaxation techniques or practices recommended during this waiting period?
Managing anxiety effectively as your procedure approaches is key to a calm and successful experience.
Techniques for Managing Anxiety:
Guideline: Use deep breathing exercises, meditation, or visualization techniques to help soothe your nerves.
Example: Try a guided meditation from an app or online resource specifically designed for pre-procedure relaxation.
Additional Recommendations:
Guideline: Engage in gentle activities such as listening to soothing music or reading a light book to keep your mind occupied.
Example: Prepare a playlist of calming music or download an audiobook ahead of time.
Utilizing these strategies can significantly reduce anxiety, helping you feel more relaxed and prepared as you head into your colonoscopy.
Morning of Procedure
Last-Minute Preparations:
Q8: Is there anything specific I should do or prepare for the morning of the procedure? Should I bring any documentation, medication lists, or ID with me to the procedure?
Morning of the Procedure:
Proper preparation on the morning of your colonoscopy sets the stage for a smooth procedure.
Last-Minute Preparations:
Guideline: Review your pre-procedure instructions to ensure all guidelines are followed, such as when to stop consuming any liquids.
What to Bring: Ensure you have your ID, insurance information, and a list of medications you’re currently taking, along with any necessary medical documentation.
Having everything in order reduces stress and prevents any last-minute hurdles as you arrive for your colonoscopy.
Post-Procedure Expectations
Recovery Timeframe:
Q9: How soon after the procedure will I be able to leave, and what are the immediate post-procedure care instructions? What are some common sensations or reactions I might experience immediately after the colonoscopy?
Understanding what to expect immediately following your colonoscopy can help you manage the recovery phase effectively.
Recovery Timeframe:
Guideline: Most patients are ready to leave 1 to 2 hours after the procedure, once the effects of sedation have lessened.
Example: You'll stay in a recovery area where nurses will monitor your initial recovery and ensure you are ready to go home safely.
Common Post-Procedure Sensations:
Guideline: You may experience feelings of bloating, gas, or cramping, which are normal as air was introduced into your colon during the procedure.
Example: Walking gently can help relieve these discomforts more quickly.
Being informed about the recovery process and what to expect afterward ensures you can manage the post-procedure phase with confidence and comfort.
For Patients with Chronic Conditions
General Concerns
Q10: As someone with a chronic condition (e.g., diabetes, heart disease), are there specific symptoms or issues I should watch out for during the 'no liquids' period?
General Concerns:
Managing a chronic condition requires careful attention, especially during the critical hours when no liquids are permitted.
Key Concerns:
Guideline: Be vigilant about any unusual symptoms such as dizziness, unusual fatigue, or palpitations, which may indicate an underlying issue exacerbated by fasting.
Example: For those with cardiac conditions, monitor for signs of chest discomfort or irregular heartbeat.
Being aware of how your body reacts during this period is crucial. Always have emergency contact numbers ready and understand when to seek medical help."
Diabetes Management
Q11: How should I manage my blood sugar levels during the 'no liquids' period, especially if I'm prone to hypoglycemia? Are there any adjustments I should make to my insulin or diabetic medication schedule in the hours leading up to the procedure?
Diabetes Management:
Diabetes requires meticulous management during the 'no liquids' phase, especially to prevent blood sugar fluctuations.
Blood Sugar Management:
Guideline: Monitor your blood sugar levels more frequently. If you're prone to hypoglycemia, discuss with your healthcare provider the possibility of adjusting your insulin or medication schedule.
Example: You might be advised to lower your insulin dose or use a short-acting insulin only.
Medication Adjustments:
Guideline: Coordinate with your endocrinologist or primary care provider to adjust medications that should not be taken on an empty stomach or require adjustment due to fasting.
Example: You may need to skip or modify doses of medications that significantly lower blood glucose, such as sulfonylureas or insulin.
Effective diabetes management during this time is vital to avoid complications. Regular monitoring and prior planning with your medical team will help maintain stable blood glucose levels.
Heart and Kidney Conditions
Q12: Given my heart/kidney condition, what precautions should I take to avoid dehydration or electrolyte imbalance during the 'no liquids' phase? Should I monitor my blood pressure more closely, and what signs should prompt me to seek immediate medical attention?
Heart and Kidney Conditions:
Individuals with heart or kidney conditions need to take extra precautions during fasting periods to prevent dehydration and electrolyte imbalance.
Dehydration and Electrolyte Imbalance:
Guideline: Be cautious about dehydration signs, such as increased thirst, dry mouth, or reduced urine output, which can affect your heart or kidney function.
Example: Have a plan for mild hydration if approved by your doctor, and know the symptoms of electrolyte imbalance like muscle cramps or changes in heartbeat.
Blood Pressure and Kidney Function Monitoring:
Guideline: If you have a heart or kidney condition, keep a close watch on your blood pressure and look out for any swelling or changes in urine color, which could indicate a problem.
Example: Use a home blood pressure monitor and check your blood pressure according to a schedule suggested by your healthcare provider.
Taking these precautions seriously will help you manage your heart or kidney condition safely during the 'no liquids' phase. Always be ready to contact your healthcare provider if you notice concerning symptoms.
Chronic GI Disorders
Q13: If I have a chronic GI disorder like Crohn's disease or ulcerative colitis, how might the 'no liquids' rule impact me differently, and how can I prepare? Are there any last-minute adjustments I should consider for my condition before the colonoscopy?
Chronic GI Disorders:
Managing a chronic GI disorder requires special consideration, especially during a period when no liquids are allowed.
Impact of 'No Liquids' Rule:
Guideline: Understand that dehydration can exacerbate symptoms of GI disorders, such as increased bowel movements or abdominal pain.
Example: Patients with Crohn's might experience more discomfort if hydration levels drop, making bowel movements more painful or difficult.
Preparation and Adjustments:
Guideline: Discuss with your gastroenterologist any specific preparations or adjustments needed, such as possibly shortening the 'no liquids' window if medically advisable.
Example: You might be allowed to take small sips of water with medication or use moisture swabs to keep your mouth moist without affecting the colonoscopy results.
Tailoring the preparation process to fit your chronic GI condition is crucial to prevent flare-ups and ensure the procedure goes smoothly. Close communication with your healthcare provider is key.
Medication Timing and Adjustments
Q14: For medications related to my chronic condition(s) that I typically take during the 'no liquids' timeframe, what alternative instructions should I follow? How can I ensure that stopping liquids won't interfere with the medications I need for my chronic conditions?
Medication Timing and Adjustments:
Adhering to medication schedules while following the 'no liquids' rule can be challenging, but it’s essential for maintaining your health during the preparation phase.
Alternative Instructions for Medication Intake:
Guideline: If your medication schedule conflicts with the 'no liquids' rule, consult your doctor about alternative dosing options or forms.
Example: Some medications may be available in dissolvable or sublingual forms that can be taken without water.
Ensuring Effective Medication Management:
Guideline: Plan ahead to adjust the timing of your medications so that they do not interfere with the fasting period.
Example: Adjust the timing of medications that are crucial for your condition, such as heart or blood pressure medicines, to earlier in the day before the 'no liquids' period begins.
Proper management of your medications is as crucial as the prep itself. Make sure to create a plan with your healthcare provider that considers both your medical needs and the requirements of the colonoscopy prep.
Transportation and Support for Chronic Conditions
Ensuring Safe Transportation
Q15: Given my chronic condition, should I arrange for medical transport or an ambulance service instead of a standard driver, especially if I live alone or lack nearby support? What information or medical supplies should my driver be aware of or have on hand in case of an emergency related to my chronic condition?
Ensuring Safe Transportation:
For patients with chronic conditions, arranging safe and appropriate transportation to and from the colonoscopy is crucial, especially when living alone or without nearby support.
Choice of Transportation:
Guideline: Consider your health stability and any potential emergency needs when choosing your mode of transportation.
Example: If you have a condition that might require immediate medical attention, such as severe diabetes or heart disease, arranging for medical transport or an ambulance service may be prudent.
Preparation for Emergencies:
Guideline: Ensure that your driver, whether a family member, friend, or medical transport professional, is informed about your condition and knows how to act in case of an emergency.
Example: Provide your driver with a list of your medications, a brief medical history, and instructions on what to do or whom to call if you experience symptoms related to your chronic condition during the trip.
Choosing the right transportation can significantly reduce the risk of complications related to your chronic condition during the colonoscopy preparation and recovery period.
Additional Support
Direct Communication with Healthcare Providers
Q16: Should I have a direct line to my healthcare provider or a specialist nurse during the 'no liquids' period in case I have questions related to my chronic condition? Is there a protocol for urgent consultations on the day of the procedure if my chronic condition exacerbates?
Additional Support and Direct Communication with Healthcare Providers:
Direct access to your healthcare provider is another key aspect of preparation, particularly during the critical hours leading up to your procedure.
Direct Line to Healthcare Providers:
Guideline: Have a direct line of communication to your healthcare provider or a designated specialist nurse during the 'no liquids' period.
Example: Keep your healthcare provider’s phone number handy, and don’t hesitate to call if you have urgent questions about your condition or the preparation process.
Protocol for Urgent Consultations:
Guideline: Understand and prepare for the protocol regarding urgent consultations on the day of the procedure, especially if there is a risk of exacerbation of your chronic condition.
Example: Ask your healthcare provider about the steps to follow if you experience a significant exacerbation of symptoms, including how to quickly get medical advice or assistance at the facility.
Maintaining a clear and direct communication pathway with your healthcare team is crucial, especially when dealing with chronic conditions. This ensures you receive the best possible care and that your concerns are addressed promptly.
T-6 Hours Before Colonoscopy Preparation User Guide
Additional Notes:
Emergency Contact: Keep your healthcare provider’s contact information readily accessible. If you experience severe symptoms, contact them immediately.
Transportation: Ensure that your driver is prepared for how long the procedure will last and knows whether they should come inside the facility or wait.
Post-Procedure Care: Make sure you understand the post-procedure care instructions as provided by the healthcare team, including how to manage any immediate side effects.
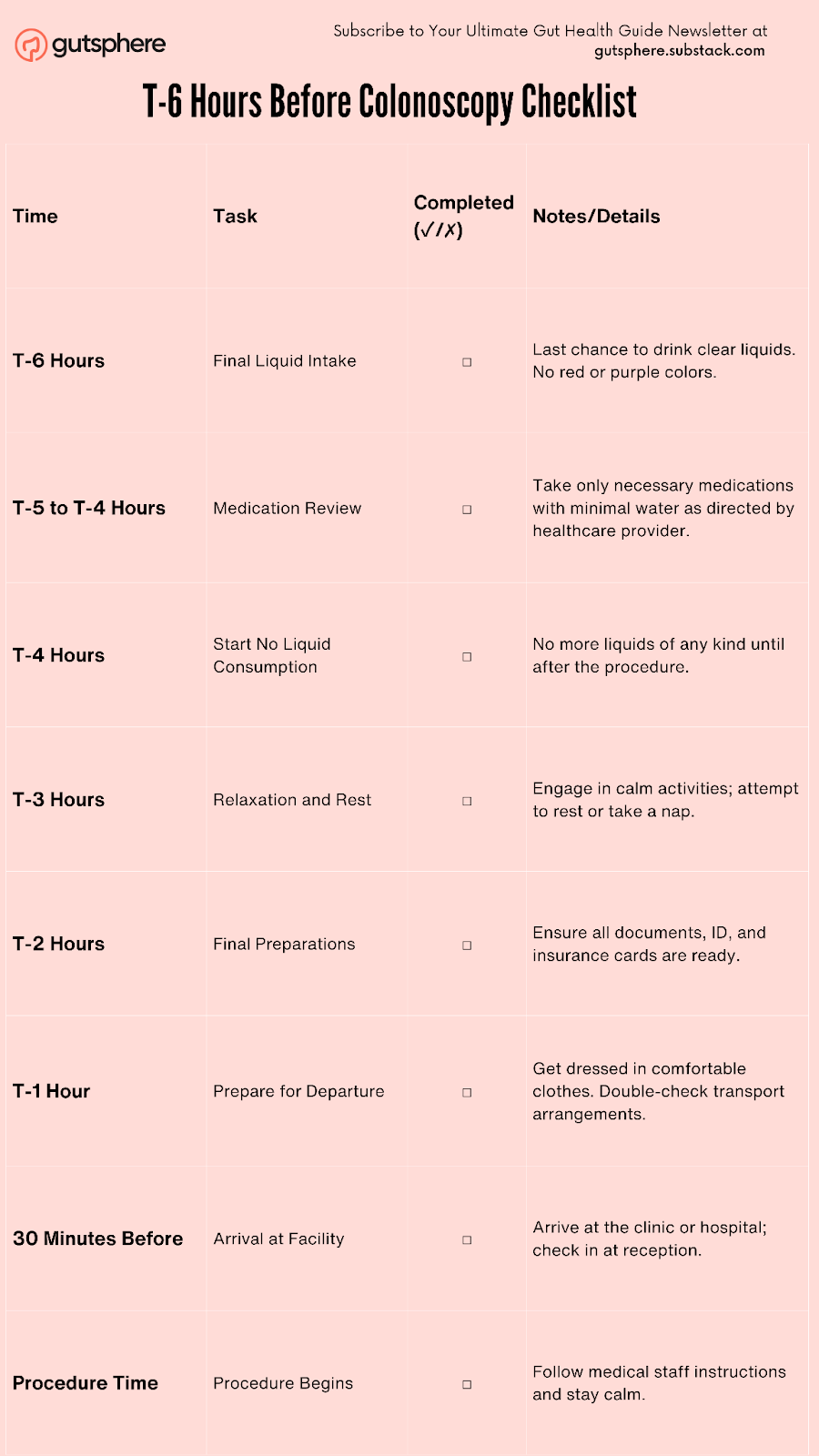
T-6 Hours Before Colonoscopy Checklist
Additional Tasks:
Emergency Contact: Make sure you have your healthcare provider's contact information handy in case of urgent questions or severe symptoms.
Reminder for Driver: Confirm that your driver understands pick-up times, procedure length, and post-procedure requirements.
Medical Supplies: If applicable, remind your driver to have any necessary medical supplies ready, especially if you have chronic conditions requiring specific care.
This checklist should be printed and kept handy as a reference during the final hours leading up to the colonoscopy, ensuring a smooth and stress-free preparation process.
Conclusion
As we conclude the T-6 Hours episode of our Colonoscopy Preparation Podcast series, I'd like to commend you on making it this far through the preparation process. Over the last few hours, we've navigated through the final and critical stages of preparation, focusing on everything from adhering strictly to the no liquid consumption rule to managing medications and ensuring you're set for a smooth procedure.
Today, we've covered essential aspects such as the importance of arriving at your procedure with a clear colon, the timing of your last liquid intake, and how to handle medications effectively during the no liquids phase. We also discussed logistical preparations to ensure that your transportation and support systems are in place and well-informed, providing a seamless transition from home to the procedure facility.
By now, your preparations are nearly complete, and you should feel confident that you've done everything possible to ensure a successful colonoscopy. Your commitment to following through with each recommended step will help optimize the effectiveness of the procedure and contribute to the most accurate outcomes.
Looking ahead to the next episode, we will be joining you post-procedure to discuss what you can expect during the recovery phase, how to manage any immediate post-procedure sensations or reactions, and long-term care following your colonoscopy. Remember, the steps you take after the procedure are just as important as those leading up to it for maintaining your health and well-being.
Thank you for your dedication to your health and for trusting us to guide you through this process. Rest assured, you are well-prepared for your upcoming colonoscopy. We look forward to supporting you through the recovery phase and beyond. Good luck, and see you on the other side of your procedure!
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
GutSphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.
References:
No Liquid Consumption
Clarification on Restrictions:
https://my.clevelandclinic.org/health/treatments/22657-colonoscopy-bowel-preparation
https://www.webmd.com/colorectal-cancer/prepare-for-colonoscopy
Medication Intake:
https://www.utmedicalcenter.org/sites/default/files/imported/wordpress/2019/02/colonoscopy_post_op_instructions_21.pdf
https://my.clevelandclinic.org/health/treatments/22657-colonoscopy-bowel-preparation
Reminder for Driver
https://my.clevelandclinic.org/health/treatments/22657-colonoscopy-bowel-preparation
https://health.usnews.com/health-care/patient-advice/articles/2017-10-10/what-to-do-about-pre-colonoscopy-anxiety
Driver’s Role and Requirements:
https://gastroconsultants.com/preparing-for-your-procedure
https://healthy.kaiserpermanente.org/washington/get-care/additional-services/gastroenterology/colon-prep
Health and Safety Concerns
https://my.clevelandclinic.org/health/treatments/22657-colonoscopy-bowel-preparation
https://doi.org/10.1136/bmjgast-2023-001193
Emergency Contacts:
https://my.clevelandclinic.org/health/treatments/22657-colonoscopy-bowel-preparation
Pre-Procedure Anxiety
https://health.usnews.com/health-care/patient-advice/articles/2017-10-10/what-to-do-about-pre-colonoscopy-anxiety
https://info.iowaradiology.com/6-tips-for-calming-your-nerves-during-colonoscopy
Morning of Procedure
https://stanfordhealthcare.org/content/dam/SHC/treatments/e/docs/colonoscopy-prep-revised-sep-6-2018.pdf
https://thewell.northwell.edu/digestive-health/colonoscopy-prep
Post-Procedure Expectations
https://www.verywellhealth.com/what-to-do-after-a-colonoscopy-796903
For Patients with Chronic Conditions
https://bmjopengastro.bmj.com/content/10/1/e001193
https://endovisionclinic.com/wp-content/uploads/2020/07/Preparation-Colonoscopy-Chronic-Constipation-2020.pdf
Transportation and Support for Chronic Conditions
https://stanfordhealthcare.org/content/dam/SHC/treatments/e/docs/colonoscopy-prep-revised-sep-6-2018.pdf