Fasting and Gut Health Connection: The Science, Benefits, and Best Practices ( Part 1/4)
Master the Art of Fasting to Enhance Your Gut Microbiome and Overall Well-being
Welcome Back, GutSphere Friends!
Welcome back to another edition of Gutsphere - Your Ultimate Companion to Gut Health! So far, we've delved into a variety of essential topics to support our journey towards a healthier gut, such as fiber, FODMAP, fermented foods, meditation, and breathing exercises.
In this edition, we're thrilled to introduce a new and exciting topic: Fasting and Gut Health Connection! Due to the extensive nature of this subject, we've decided to split it into four parts to ensure that each aspect is covered thoroughly and coherently.
Here's the breakdown of the four parts:
Part 1: Introduction to Fasting and Gut Health
What is fasting?
Basic Understanding of Fasting and Gut Health
What's the Science behind fasting?
What are the different types of fasting, and how do they affect gut health differently?
Fasting Timeline: What Happens to our Body During Different Stages of Fasting?
Part 2: Fasting's Effects on Gut Health and Microbiome
How does fasting influence the diversity and composition of the gut microbiome?
What are the short-term and long-term effects of fasting on gut health and overall health?
Factors Affecting Fasting and Gut Health
Gut Health Mechanisms and Fasting
Part 3: Fasting Practices, Optimization, and Personalization
Fasting Practices for Beginners, Intermediate, and Advanced levels
How does the re-feeding period after fasting influence gut microbiome composition and gut health?
How does the duration and frequency of fasting periods impact gut health outcomes?
What role does diet play in conjunction with fasting to optimize gut health benefits?
Part 4: Addressing Concerns, Monitoring Effects, and Fasting as a Therapeutic Intervention
Contradictions, Myths, Criticisms, and Negative effects of fasting
Are there any populations for whom fasting is contraindicated due to potential negative effects on gut health?
Monitoring and Measuring the Effects of Fasting on Gut Health
Integrating Fiber, Fermented Foods, FODMAP, and Fasting for Optimal Gut Health
Fasting as a Therapeutic Intervention
The future of fasting as a therapy
Research papers we are reading
In Part 1, we'll explore the basics of fasting and how it's connected to gut health. Let's get started!
What is fasting?
Fasting, a practice rooted in our evolutionary, historical, religious, and cultural backgrounds, refers to the voluntary abstinence from food or drink for a specific period. Let us take a journey through time to explore how fasting has evolved and become an essential part of our lives.
In our evolutionary past, our ancestors had to endure long periods without food due to the unpredictable nature of their environment. This necessity to adapt to food scarcity shaped our bodies' ability to switch between burning glucose and stored fat for energy, allowing us to survive and even thrive during periods of fasting.
Throughout history, fasting has been a part of various religious and cultural practices. In Christianity, for example, fasting has long been associated with penance and spiritual growth, with believers abstaining from food on specific days like Ash Wednesday and Good Friday. Similarly, Muslims fast from dawn until sunset during the month of Ramadan to strengthen their spiritual connection and self-discipline. Hindus, Buddhists, and followers of other religious traditions also practice fasting for spiritual and physical purification.
Different cultures have also embraced fasting as a way to promote health, self-discipline, and mental clarity. In ancient Greece, the philosopher and mathematician Pythagoras reportedly fasted for 40 days to improve mental acuity. Traditional Chinese medicine has also used fasting as a therapeutic tool for centuries.
Modern science began to consider fasting as beneficial for health in the early 20th century when researchers discovered that fasting could help treat epilepsy. Since then, scientific interest in fasting has grown exponentially. Research now shows that fasting can promote weight loss, improve metabolic health, enhance cognitive function, and even extend lifespan.
Today, we continue to explore the potential benefits of fasting and incorporate it into our lives in various ways. From intermittent fasting to prolonged fasting, we strive to understand and optimize this ancient practice for our modern needs. As we delve deeper into fasting's mechanisms and potential, we can better harness its power to improve our health and well-being.
In today’s edition, we will deep dive into how fasting affects gut health. We will structure the content in Q&A format so that it is easier to grasp.
Let’s begin with the basic understanding of Fasting and Gut Health.
Basic Understanding of Fasting and Gut Health
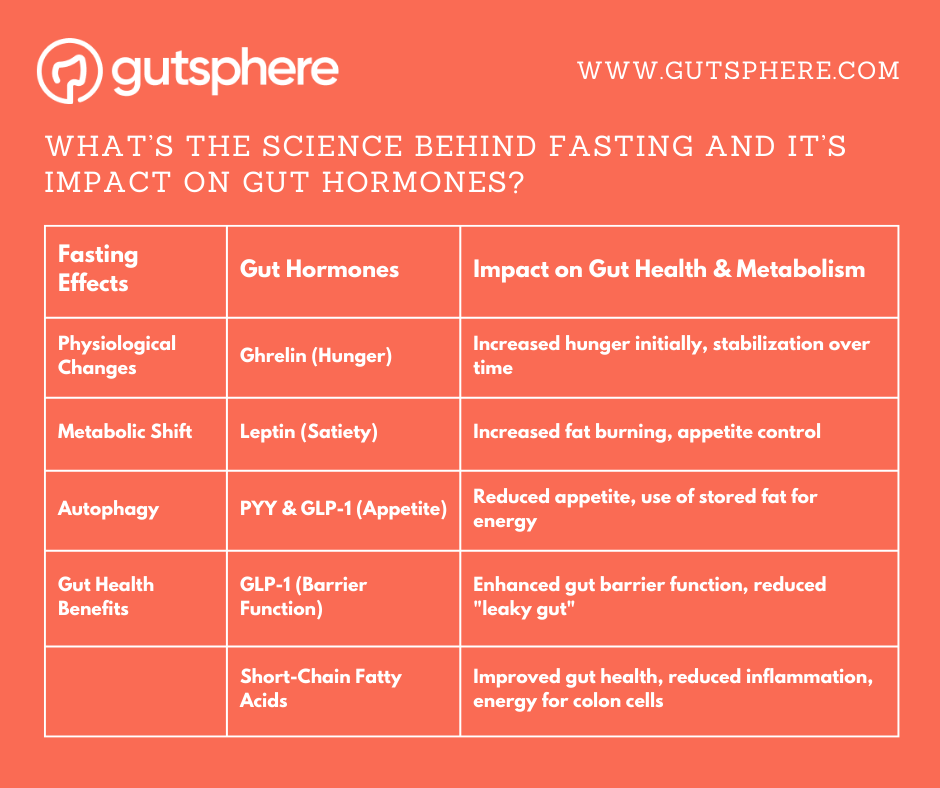
What’s the Science behind fasting and it’s impact on gut hormones?
When we fast, our bodies undergo a series of physiological changes to maintain energy levels and adapt to the absence of incoming nutrients. One of the key adaptations during fasting involves alterations in the production of certain gut hormones, which play crucial roles in maintaining gut health, regulating appetite, and controlling metabolism.
During fasting, the body's metabolic state shifts from the fed state to the fasted state. In the fed state, glucose from food is used as the primary source of energy. The excess glucose is stored in the liver and muscles as glycogen. However, when the body enters the fasted state, it begins to use stored energy from glycogen and then from stored fat for energy. This metabolic shift is accompanied by a decrease in insulin levels, which allows the body to access stored energy through a process known as lipolysis. During lipolysis, stored fat is broken down into fatty acids and glycerol, which can be used for energy.
As fatty acids are broken down for energy, they are converted into ketones, which can be used by the body's tissues, including the brain, as an alternative source of energy. This metabolic state is known as ketosis and is a hallmark of fasting. The ketones produced during fasting have been shown to have various health benefits, including neuroprotective effects and improved cognitive function.
Fasting also triggers a cellular recycling process called autophagy, wherein damaged and dysfunctional cellular components are broken down and recycled for energy or rebuilt. This process is essential for maintaining cellular health, preventing the accumulation of damaged cellular components, and promoting the efficient functioning of cells. Autophagy has been linked to anti-aging effects, as well as protection against various diseases, such as neurodegenerative disorders and cancer.
When it comes to gut hormones, fasting has a significant impact on their production and function. Some of the key gut hormones affected by fasting include ghrelin, leptin, peptide YY (PYY), and glucagon-like peptide-1 (GLP-1).
Ghrelin, often referred to as the "hunger hormone," is produced primarily in the stomach and stimulates appetite. During fasting, ghrelin levels tend to increase, signaling the body that it's time to eat. This rise in ghrelin can lead to an increased sensation of hunger during fasting periods. However, as we continue to fast, our bodies gradually adapt, and ghrelin levels tend to stabilize, reducing hunger sensations over time.
Leptin, on the other hand, is the "satiety hormone," which helps signal to the brain that we've had enough to eat. Leptin is primarily produced by fat cells and helps regulate energy balance by inhibiting hunger. During fasting, leptin levels may decrease, leading to an increased sense of hunger. However, the drop in leptin levels can also promote increased fat burning, as the body switches to stored fat for energy.
PYY and GLP-1 are other gut hormones that play a role in appetite regulation and are influenced by fasting. Both hormones are released by cells in the intestines in response to food intake and promote feelings of fullness. During fasting, levels of PYY and GLP-1 may decrease initially but tend to stabilize as the body adapts to the fasting state. These adaptations may help reduce appetite and encourage the body to use stored fat for energy.
In addition to appetite regulation, gut hormones are involved in various other functions, such as glucose homeostasis, gastrointestinal motility, and the regulation of the gut microbiome. Research suggests that fasting may help improve insulin sensitivity, modulate inflammation, and promote the growth of beneficial gut bacteria. These changes can have a positive impact on overall gut health and contribute to the potential health benefits of fasting.
For example, fasting has been shown to enhance the production of short-chain fatty acids (SCFAs) by gut bacteria. SCFAs, such as acetate, propionate, and butyrate, play important roles in maintaining gut barrier function, modulating the immune system, and providing energy to colon cells. By promoting the growth of beneficial gut bacteria and increasing SCFA production, fasting may help improve gut health and reduce the risk of various gut-related disorders, such as inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS).
Furthermore, fasting has been shown to affect the production of gut hormones involved in intestinal barrier function and permeability. For instance, GLP-1 has been found to improve gut barrier function by enhancing the expression of tight junction proteins, which are essential for maintaining the integrity of the gut lining. This, in turn, can help protect against the development of "leaky gut" and associated health issues, such as chronic inflammation and autoimmune diseases.
In conclusion, fasting can have a significant impact on the production of gut hormones, which play essential roles in maintaining gut health, regulating appetite, and controlling metabolism. As we adapt to fasting, our bodies undergo various changes, including alterations in gut hormone levels, which can ultimately lead to improvements in gut health and overall well-being.
What are the different types of fasting, and how do they affect gut health differently?
When exploring the different types of fasting and their impact on gut health, we can identify several common fasting methods. As we go through these methods, it's essential to remember that individual results may vary, and what works for one person might not work for another. Here are the various types of fasting and their potential effects on gut health:
Intermittent Fasting (IF)
Method: Alternating between periods of eating and fasting within a day or a week. A popular form is the 16:8 method, with a 16-hour fast and an 8-hour eating window.
Impact on Gut Health: Promotes gut microbiome diversity and enhances the production of short-chain fatty acids (SCFAs), which serve as an energy source for colon cells and play a role in reducing inflammation.
Alternate-Day Fasting (ADF)
Method: Alternating between days of normal eating and complete or partial fasting.
Impact on Gut Health: Might lead to more pronounced changes in gut microbiome composition and increased production of SCFAs, though adherence can be more challenging compared to IF.
Periodic Fasting (PF)
Method: Fasting for extended periods, typically ranging from 2 to 5 days.
Impact on Gut Health: Induces a more profound shift in the gut microbiome, promotes autophagy (a cellular self-cleaning process), and stimulates the production of gut-protective compounds. Be cautious during the refeeding phase to prevent potential negative effects on gut health.
Time-Restricted Eating (TRE)
Method: Eating within a specific time window each day, often aligning with the circadian rhythm.
Impact on Gut Health: Helps regulate gut hormones and improves gut barrier function, contributing to better gut health.
Religious Fasting
Method: Fasting practices incorporated into various religions, such as Ramadan in Islam or Lent in Christianity. These fasts can vary in duration and intensity.
Impact on Gut Health: Can lead to similar gut health benefits as other fasting methods, such as improved gut microbiome diversity and increased SCFA production.
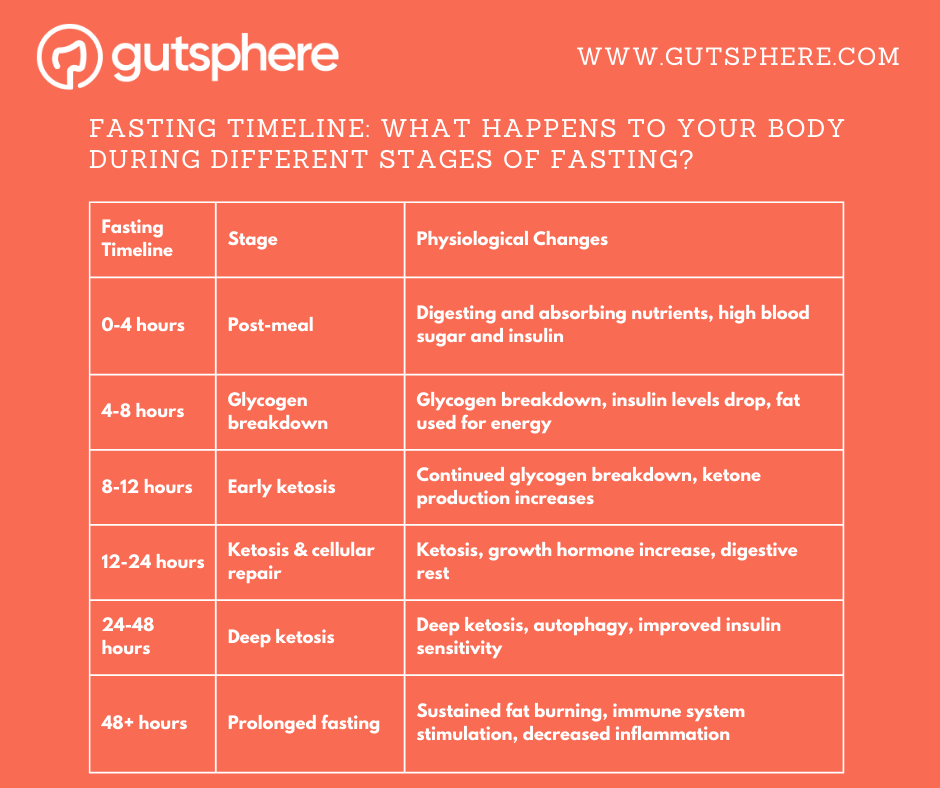
We are curious about what happens to our body at different fasting timelines. It's important to note that everyone's body will respond differently to fasting, and these timeframes are just general guidelines.
Fasting Timeline: What Happens to Your Body During Different Stages of Fasting?
0-4 hours: After the last meal, the body is still digesting and absorbing nutrients. Blood sugar and insulin levels are high, and the body is using glucose from food as its primary source of energy.
4-8 hours: The body has used up the glucose from the last meal and begins to break down stored glycogen in the liver and muscle tissue to maintain blood sugar levels. Insulin levels start to drop, and the body begins to shift towards using stored fat as an energy source.
8-12 hours: The body continues to break down glycogen stores for energy. The body enters a state of ketosis, where it begins to break down stored fat for energy, and ketone levels increase.
12-24 hours: Ketone levels continue to rise as the body shifts towards using stored fat for energy. Growth hormone levels increase, which can help to preserve lean muscle mass. The digestive system rests, allowing the body to focus on cellular repair and regeneration.
24-48 hours: The body is in a deep state of ketosis, and the production of ketones increases. Autophagy, a cellular recycling process, ramps up, which can help to remove damaged cells and improve cellular health. Insulin levels continue to decrease, and the body becomes more insulin-sensitive.
48+ hours: The body continues to burn stored fat for energy, and ketone levels remain high. The immune system may be stimulated, and stem cell production increases. Prolonged fasting can also lead to a decrease in inflammation and oxidative stress.
When we fast, we create changes in the gut environment that can impact the diversity and composition of the gut microbiome. The duration of the fast is an important factor that can determine how the gut microbiome responds.
Let's take a closer look at how different stages and timelines of fasting can affect the gut microbiome in Part 2.
We hope you found this introduction to fasting and its connection to gut health insightful. As we've seen, there's more to fasting than just going without food. But wait, there's more! In Part 2, we'll delve deeper into the effects of fasting on gut health and the microbiome. Stay tuned—you won't want to miss it!
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
If you haven’t already subscribed then our sincere request, please subscribe.
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
gutsphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.