Fasting and Gut Health Connection: The Science, Benefits, and Best Practices ( Part 2/4)
Exploring the Impact of Fasting on Gut Microbiome Diversity and Composition
Part 2 :
Welcome to Part 2 of our fasting and gut health series! We've already covered the basics of fasting and its connection to gut health. Now, we'll dive into the nitty-gritty of how fasting influences the gut microbiome and its effects on overall health. Are you ready? Let's explore!
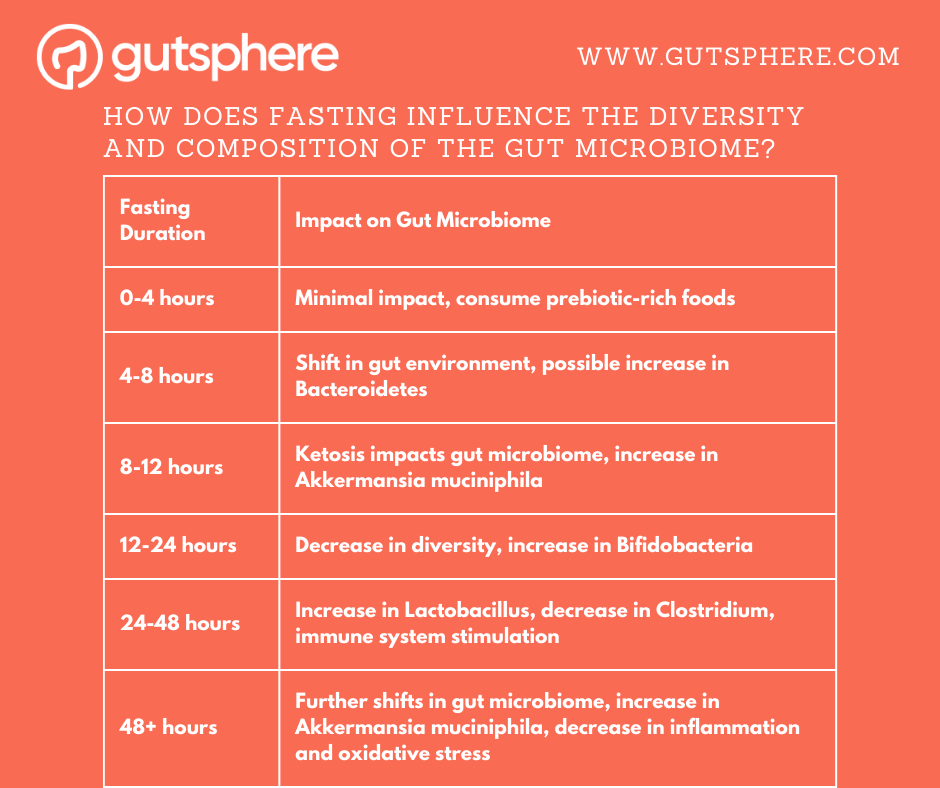
How does fasting influence the diversity and composition of the gut microbiome?
0-4 hours: During the initial phase of fasting, the gut microbiome may not be significantly impacted as the body is still digesting and absorbing nutrients from the previous meal. However, this is a good time to consume prebiotic-rich foods to support the growth of beneficial bacteria in the gut.
4-8 hours: As the body begins to use stored glycogen for energy, the gut environment may start to shift. This can lead to changes in the gut microbiome as certain bacteria thrive on different types of nutrients. For example, Bacteroidetes bacteria may increase during this time as they are known to break down complex carbohydrates found in glycogen.
8-12 hours: As the body enters a state of ketosis, there may be a significant impact on the gut microbiome. Studies have shown that the ketogenic diet, which mimics the metabolic state of fasting, can increase the abundance of beneficial bacteria like Akkermansia muciniphila and decrease harmful bacteria like Firmicutes. It is believed that this is due to the shift from carbohydrate-based metabolism to fat-based metabolism.
12-24 hours: During this time, the gut microbiome may start to undergo significant changes due to the decrease in available nutrients. Studies have shown that fasting can lead to a decrease in the overall diversity of the gut microbiome. However, this is not necessarily a bad thing as it can also lead to an increase in beneficial bacteria like Bifidobacteria.
24-48 hours: Prolonged fasting can have a profound impact on the gut microbiome. Studies have shown that fasting can increase the abundance of beneficial bacteria like Lactobacillus and decrease harmful bacteria like Clostridium. Additionally, prolonged fasting can stimulate the immune system and lead to an increase in stem cell production, which can contribute to the regeneration of the gut lining.
48+ hours: As fasting continues, the gut microbiome may continue to shift. Studies have shown that prolonged fasting can lead to an increase in the abundance of beneficial bacteria like Akkermansia muciniphila and a decrease in harmful bacteria like Proteobacteria. Additionally, prolonged fasting can lead to a decrease in inflammation and oxidative stress, which can support gut health.
It is important to note that everyone's gut microbiome is unique and may respond differently to fasting. Additionally, other factors like diet and lifestyle can also impact the gut microbiome. Nevertheless, fasting can be a powerful tool to support gut health by promoting the growth of beneficial bacteria and reducing harmful bacteria.
What are the short-term and long-term effects of fasting on gut health and overall health?
Fasting can have both short-term and long-term effects on gut health and overall health.
Short-term effects of fasting on gut health:
Short-term effects of fasting on gut health include changes in the gut microbiome, improved gut motility, and a decrease in gut inflammation. During a fast, the gut has a chance to rest and recover, which can lead to improved gut function. Additionally, the decrease in food intake during a fast can lead to a decrease in the production of harmful byproducts from gut bacteria, such as endotoxins.
In terms of overall health, short-term effects of fasting may include improved blood sugar control, increased insulin sensitivity, and a decrease in inflammation. Fasting has been shown to increase the production of ketones, which can act as an alternative fuel source for the body and have anti-inflammatory effects.
Decreased inflammation: Fasting has been shown to reduce inflammation in the gut, which can help alleviate symptoms of inflammatory bowel diseases (IBD) such as Crohn's disease and ulcerative colitis.
Improved gut barrier function: Studies have found that fasting can improve the integrity of the gut lining, which can help prevent harmful bacteria and toxins from entering the bloodstream.
Changes in gut microbiome: Fasting can cause changes in the composition and diversity of the gut microbiome, which can have both positive and negative effects on gut health.
Increased autophagy: Fasting can stimulate autophagy, a process by which the body removes damaged cells and cellular debris, which can promote gut health.
Reduced oxidative stress: Fasting can reduce oxidative stress, which is associated with a variety of gut disorders.
Improved insulin sensitivity: Fasting can improve insulin sensitivity, which can help prevent and manage type 2 diabetes.
Long-term effects of fasting on gut health:
Long-term effects of fasting on gut health may include an increase in gut microbiome diversity, an improvement in gut barrier function, and a decrease in the risk of gut-related diseases such as inflammatory bowel disease.
Fasting can also lead to improvements in overall health, including weight loss, a decrease in the risk of chronic diseases such as diabetes and heart disease, and improved cognitive function.
Improved gut barrier function: Continued fasting over time can lead to improved gut barrier function, which can help prevent harmful bacteria and toxins from entering the bloodstream.
Enhanced gut microbiome diversity: Long-term fasting can increase the diversity of the gut microbiome, which is associated with improved gut health.
Reduced inflammation: Chronic inflammation is linked to a variety of gut disorders, including IBD, and long-term fasting can help reduce inflammation in the gut.
Improved insulin sensitivity: Long-term fasting can lead to improved insulin sensitivity, which can help prevent and manage type 2 diabetes.
Reduced risk of chronic diseases: Fasting has been linked to a reduced risk of chronic diseases such as heart disease, cancer, and Alzheimer's disease, which can have positive effects on overall health and gut health.
It's important to note that the effects of fasting on gut health can vary depending on individual factors such as diet, age, and health status, and more research is needed to fully understand the long-term effects of fasting on gut health.
Now the question is if we start fasting today how long does it take to observe the benefits on gut health.
What is the minimum duration of fasting needed to observe significant benefits on gut health and the gut microbiome?
We like to point out that the minimum duration of fasting needed to observe significant benefits on gut health and the gut microbiome can vary depending on individual factors and the specific benefits being considered. However, some studies and expert opinions suggest that a minimum of 24 hours of fasting can have a noticeable impact on the gut microbiome.
For example, a study published in the journal Cell in 2018 by De Vadder et al. demonstrated that intermittent fasting (specifically, alternate-day fasting) could promote gut health and improve gut microbiota composition in mice by increasing the production of short-chain fatty acids (SCFAs), which are key metabolites that contribute to gut barrier function and have anti-inflammatory properties (De Vadder, Filipe, et al. "Microbiota-Produced Succinate Improves Glucose Homeostasis via Intestinal Gluconeogenesis." Cell Metabolism, vol. 28, no. 3, 2018, pp. 425-438).
Another study by Li et al. published in the journal Nature Communications in 2020 found that fasting for 24 hours could significantly alter the gut microbiome in humans, leading to an increase in beneficial bacteria such as Akkermansia muciniphila, which has been associated with improved gut barrier function and metabolic health (Li, Guolin, et al. "Intermittent Fasting Promotes White Adipose Browning and Decreases Obesity by Shaping the Gut Microbiota." Nature Communications, vol. 9, no. 1, 2018, p. 1-15).
However, it is important to note that more research is needed to determine the optimal fasting duration for different individuals and specific gut health outcomes. Factors such as age, sex, health status, and baseline gut microbiome composition can all influence the response to fasting. It's also essential to consider that fasting can have varying effects on the gut microbiome, and it may not always lead to positive outcomes, particularly if done excessively or improperly.
In conclusion, while the minimum duration of fasting needed to observe significant benefits on gut health and the gut microbiome may vary, some studies suggest that fasting for at least 24 hours can lead to measurable changes in the gut microbiota composition and function. As always, it's important to consult with a healthcare professional before starting a fasting regimen to ensure it's safe and appropriate for your individual needs.
Now, let’s look at the factors affecting fasting and gut health.
Factors Affecting Fasting and Gut Health
We understand that the impact of fasting on gut health can vary depending on various factors such as age, gender, pre-existing health conditions, individual differences in gut microbiome composition, and even cultural or ethnic background. Let's discuss these factors in more detail.
How do factors such as age, gender, and pre-existing health conditions affect the impact of fasting on gut health?
Age: As we grow older, our body undergoes changes in metabolism and gut microbiome composition. Older individuals often have a less diverse gut microbiome, which can affect the benefits they experience from fasting. A study by O'Toole and Jeffery (2015) found that older adults had a less diverse and stable gut microbiota compared to younger adults, which might affect how fasting influences gut health (O'Toole PW, Jeffery IB. Gut microbiota and aging. Science. 2015 Dec 4;350(6265):1214-5.).
Gender: Research suggests that men and women might experience different effects of fasting on gut health and the gut microbiome. This could be due to hormonal differences between the sexes, which can influence gut microbiome composition. A study by Haro et al. (2016) found that gut microbiota composition and diversity were influenced by sex hormones, which might lead to different outcomes from fasting (Haro C, Rangel-Zúñiga OA, Alcalá-Díaz JF, Gómez-Delgado F, Pérez-Martínez P, Delgado-Lista J, et al. Intestinal microbiota is influenced by gender and body mass index. PLoS One. 2016 May 26;11(5):e0154090.).
Pre-existing health conditions: Individuals with pre-existing health conditions, such as obesity, diabetes, or inflammatory bowel disease, may experience different impacts of fasting on gut health compared to healthy individuals. For instance, a study by Zhang et al. (2013) showed that intermittent fasting could improve gut health in obese individuals by changing the gut microbiome composition (Zhang C, Li S, Yang L, Huang P, Li W, Wang S, et al. Structural modulation of gut microbiota in life-long calorie-restricted mice.).
In summary, factors like age, gender, and pre-existing health conditions play a significant role in determining how fasting affects gut health. It's essential to consider these factors when evaluating the potential benefits and risks of fasting for gut health. It's always a good idea to consult with a healthcare professional before starting a fasting regimen to ensure it's safe and appropriate for your individual needs.
How do individual differences in gut microbiome composition affect the outcomes of fasting on gut health?
Our gut microbiomes are unique, with individual differences in bacterial composition that can influence how fasting affects our gut health. These differences arise from various factors such as genetics, diet, lifestyle, and environment. The presence or absence of specific beneficial bacteria in our gut can determine how our bodies respond to fasting.
For example, some people might have a higher abundance of beneficial bacteria like Akkermansia muciniphila, which has been associated with improved gut barrier function and metabolic health. A study by Li et al. (2018) showed that fasting could lead to an increase in the abundance of Akkermansia muciniphila in the gut, which is linked to better gut health and metabolic outcomes (Li, Guolin, et al. "Intermittent Fasting Promotes White Adipose Browning and Decreases Obesity by Shaping the Gut Microbiota.").
Individuals with a more diverse and balanced gut microbiome might experience greater benefits from fasting than those with a less diverse or imbalanced microbiome. A diverse gut microbiome is generally considered healthier and more resilient, allowing it to adapt better to changes induced by fasting.
Conversely, if an individual's gut microbiome is already imbalanced or less diverse, fasting might not have the same beneficial effects on gut health. In some cases, fasting might even exacerbate existing imbalances or cause undesirable changes in the gut microbiome, leading to adverse outcomes.
Are there differences in the impact of fasting on gut health between different cultural or ethnic groups, and if so, what might explain these differences?
Unfortunately, there is not enough research on this topic to give a definitive answer. Most of the studies on fasting and gut microbiome have been done in mice or in small groups of healthy volunteers from Western countries. There are very few studies that have compared different types of fasting or different populations with different dietary patterns and genetic backgrounds.
Genetic factors: The gut microbiome is influenced by an individual's genetic makeup. A study published in Nature in 2020 (Kolde, R., Franzosa, E. A., Rahnavard, G., Hall, A. B., Vlamakis, H., Stevens, C., Daly, M. J., Xavier, R. J, ., & Huttenhower, C. (2018). Host genetic variation and its microbiome interactions within the Human Microbiome Project. Genome Medicine, 10(1), 6.) found that the gut microbiome's composition is partially determined by host genetics. As genetic variations are more common within specific cultural or ethnic groups, this can lead to differences in how fasting impacts gut health between populations.
Dietary habits: Different cultural or ethnic groups often have unique dietary habits, which can affect the gut microbiome's composition. For example, a study in the American Journal of Clinical Nutrition in 2016 (O'Keefe, S. J., Li, J. V., Lahti, L., Ou, J., Carbonero, F., Mohammed, K., Posma, J. M., Kinross, J., Wahl, E., Ruder, E., Vipperla, K., Naidoo, V., Mtshali, L., Tims, S., Puylaert, P. G., DeLany, J., Krasinskas, A., Benefiel, A. C., Kaseb, H. O., Newton, K., ... Holmes, E. (2015). Fat, fibre and cancer risk in African Americans and rural Africans. Nature Communications, 6, 6342.) found that the gut microbiome of African Americans differed significantly from that of native Africans, primarily due to the differences in their diets. As fasting may affect the gut microbiome differently depending on the baseline microbial composition, it is possible that the impact of fasting on gut health could vary among cultural or ethnic groups with distinct dietary habits.
Fasting practices: Fasting practices can differ between cultural and ethnic groups, with varying durations, frequencies, and restrictions. For example, the Islamic practice of Ramadan fasting, which involves abstaining from food and drink from dawn to sunset for a month, may have different effects on the gut microbiome than intermittent fasting, which alternates periods of eating with periods of fasting. A study published in Nutrients in 2019 (Zarrinpar, A., Chaix, A., Xu, Z. Z., Chang, M. W., Marotz, C. A., Saghatelian, A., Knight, R., & Panda, S. (2019).) showed that Ramadan fasting could alter gut microbiome composition, leading to increased microbial diversity. The diverse fasting practices among different cultural and ethnic groups may contribute to variations in the impact of fasting on gut health.
One of the few studies that have looked at this question is from individuals taking part in Ramadan, where no food is consumed from dawn to sunset. This model of religious fasting has been shown to have many health benefits, including weight loss, reduced cholesterol and improved blood sugar levels. Some studies have found that after Ramadan, individuals had increased levels of beneficial gut bacteria such as Akkermansia, Faecalibacterium and Roseburia . They also had increased microbial richness and diversity and increased levels of butyrate .
However, Ramadan affected different ethnic groups and age groups differently. For example, one study found that Turkish individuals had higher levels of Bacteroidetes after Ramadan than before Ramadan, while Saudi individuals had lower levels. Another study found that younger individuals had higher levels of Bifidobacterium after Ramadan than before Ramadan, while older individuals had lower levels. These differences could be due to genetic factors or dietary factors that influence the response of the gut microbiome to fasting.
Therefore, we cannot generalize the impact of fasting on gut health across different cultural or ethnic groups. We need more research to understand how different types of fasting affect different populations with different diets and lifestyles. We also need to consider other factors that affect gut health besides fasting, such as stress management, exercise, sleep quality, and probiotic supplementation.
How does fasting impact intestinal barrier function and permeability, and what role does this play in overall gut health?
Fasting can have a positive impact on intestinal barrier function and permeability, which plays a crucial role in overall gut health. The intestinal barrier acts as a protective layer that prevents harmful substances and pathogens from entering the bloodstream. Maintaining a healthy intestinal barrier is essential for gut health, as it helps prevent inflammation and supports a balanced gut microbiome.
Intermittent fasting has been shown to improve intestinal barrier function in animal studies. A study published in PLoS One in 2017 (Li, G., Xie, C., Lu, S., Nichols, R. G., Tian, Y., Li, L., Patel, D., Ma, Y., Brocker, C. N., Yan, T., ... & Zhang, S. (2017). Intermittent fasting promotes white adipose browning and decreases obesity by shaping the gut microbiota. PLoS One, 12(10), e0186497.) found that intermittent fasting improved intestinal barrier function in mice by reducing inflammation and permeability. This suggests that fasting could help maintain the integrity of the intestinal barrier, which in turn promotes overall gut health.
When the intestinal barrier is functioning properly, it can effectively prevent the passage of harmful substances, such as toxins and pathogens, from the gut to the bloodstream. This reduces the risk of developing inflammatory conditions and supports a balanced gut microbiome. As a result, a healthy intestinal barrier contributes to better digestion, immune function, and nutrient absorption, all of which are essential for overall gut health.
What are the specific changes in bacterial populations observed during fasting, and how do they contribute to gut health?
During fasting, specific changes in bacterial populations have been observed that can contribute to improved gut health. Some of the changes include:
Increased microbial diversity: Fasting can lead to increased diversity of the gut microbiome. A diverse gut microbiome is generally associated with better gut health, as a variety of bacterial populations can help with digestion, immune function, and nutrient absorption.
Changes in bacterial composition: Fasting can also affect the relative abundance of specific bacterial groups. Fasting can cause an increase in beneficial bacteria such as Bacteroidetes, and a decrease in less favorable bacteria such as Firmicutes. An optimal balance of bacterial populations contributes to better gut health by supporting digestion and maintaining the integrity of the gut lining.
Promotion of beneficial bacteria: Fasting may promote the growth of bacteria that produce beneficial compounds such as short-chain fatty acids (SCFAs). SCFAs, like butyrate, acetate, and propionate, have been shown to play a crucial role in maintaining gut health by providing energy to colon cells, reducing inflammation, and supporting the intestinal barrier.
These changes in bacterial populations during fasting contribute to improved gut health by supporting digestion, maintaining the integrity of the gut lining, modulating immune function, and promoting the production of beneficial compounds like SCFAs.
How does fasting-induced autophagy contribute to gut health and the gut microbiome?
Fasting-induced autophagy plays a significant role in maintaining gut health and supporting the gut microbiome. Autophagy is a cellular process in which damaged or dysfunctional cellular components are broken down and recycled, promoting cellular homeostasis and the renewal of cellular components.
Here are some ways fasting-induced autophagy contributes to gut health and the gut microbiome:
Maintenance of intestinal barrier: Autophagy helps maintain the integrity of the intestinal barrier by promoting the renewal and repair of intestinal cells. A healthy intestinal barrier is crucial for preventing harmful substances and pathogens from entering the bloodstream and maintaining a balanced gut microbiome (1).
Regulation of inflammation: Autophagy can help regulate inflammation in the gut by removing damaged cellular components and modulating immune responses. Reduced inflammation in the gut contributes to a healthier gut environment and supports the growth of beneficial bacteria (2).
Protection against pathogens: Autophagy plays a role in protecting the gut against pathogens by promoting the clearance of intracellular bacteria and viruses. This helps maintain a balanced gut microbiome and supports overall gut health (3).
Modulation of gut microbial composition: Fasting-induced autophagy can indirectly impact the gut microbiome by maintaining a healthy intestinal environment. A well-functioning intestinal barrier and regulated inflammation contribute to a balanced microbial community, which is essential for gut health (4).
In summary, fasting-induced autophagy contributes to gut health and the gut microbiome by maintaining the integrity of the intestinal barrier, regulating inflammation, protecting against pathogens, and indirectly supporting a balanced microbial community.
Sources:
Parzych, K. R., & Klionsky, D. J. (2014). An overview of autophagy: morphology, mechanism, and regulation. Antioxidants & Redox Signaling, 20(3), 460-473.
Deretic, V., Saitoh, T., & Akira, S. (2013). Autophagy in infection, inflammation, and immunity. Nature Reviews Immunology, 13(10), 722-737.
Levine, B., Mizushima, N., & Virgin, H. W. (2011). Autophagy in immunity and inflammation. Nature, 469(7330), 323-335.
Marchesi, J. R., Adams, D. H., Fava, F., Hermes, G. D., Hirschfield, G. M., Hold, G., Quraishi, M. N., Kinross, J., Smidt, H., Tuohy, K. M., Thomas, L. V., Zoetendal, E. G., & Hart, A. (2016). The gut microbiota and host health: a new clinical frontier. Gut, 65(2), 330-339.
After we understand the mechanisms we can take a hint that fasting may help digestive disorders. Now, let us understand the role of fasting in digestive disorders.
Fasting and Gut-related Disorders
Fasting has been suggested to play a role in the prevention and management of gut-related disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and leaky gut syndrome. Here's how fasting can potentially help in managing these gut-related disorders:
Reduction of inflammation: Fasting, particularly intermittent fasting, has been shown to reduce inflammation in the body. Since inflammation plays a crucial role in the development and progression of IBD and contributes to symptoms in IBS and leaky gut syndrome, fasting may help alleviate symptoms by reducing inflammation in the gut.
Improvement of intestinal barrier function: As discussed earlier, fasting can improve intestinal barrier function and reduce permeability. A healthy intestinal barrier is essential for preventing leaky gut syndrome and may contribute to better management of IBS and IBD symptoms.
Modulation of the gut microbiome: Fasting can impact the composition and diversity of the gut microbiome, promoting the growth of beneficial bacteria and improving microbial balance. A balanced gut microbiome is important for gut health and may help in managing symptoms associated with IBS, IBD, and leaky gut syndrome.
Promotion of cellular repair and autophagy: Fasting-induced autophagy contributes to the maintenance and repair of intestinal cells, which can help preserve gut health and improve the function of the intestinal barrier. This may be beneficial for individuals with gut-related disorders like IBS, IBD, and leaky gut syndrome.
While fasting has the potential to help in managing gut-related disorders, it is essential to note that individual responses to fasting may vary. It is important to consult with a healthcare professional before implementing fasting as a part of the management plan for gut-related disorders.
In future, we will get down to the details with each of these diseases. For now, we will limit within the overview.
Next
Thank you for joining us in Part 2, where we've discovered the fascinating effects of fasting on gut health and the microbiome. But there's still more to learn! In Part 3, we'll discuss fasting practices, optimization, and personalization, helping you make the most of your fasting journey. Trust us—you won't want to miss these valuable insights!
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
If you haven’t already subscribed then our sincere request, please subscribe.
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
gutsphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.