FODMAP Masterclass for Gut Health(Part 1/3)
Unraveling the Science, Strategies, and Sustenance for Optimal Gut Health
Part 1
Welcome Back, GutSphere Friends
Welcome to the latest edition of our gutsphere newsletter, where we continue our deep dive into gut health and provide practical tips, scientific insights, and tools to help us all live our best, gut-friendly lives. Over the course of this series, we have explored various aspects of gut health, including the importance of fiber and the benefits of fermented foods. Now, we're ready to tackle the fascinating world of FODMAPs.
In this comprehensive guide, we'll first lay the groundwork by defining FODMAPs and their various categories. We'll then explore the role they play in digestion, absorption, and gut microbiome health. To help us make informed dietary choices, we'll identify high- and low-FODMAP foods, and discuss how FODMAPs impact digestive disorders such as Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD), and Small Intestinal Bacterial Overgrowth (SIBO).
As we dig into the science behind the low-FODMAP diet, we'll examine the latest research on its impact on gut health and uncover the mechanisms of action that influence gut microbiome and symptoms. We'll also discuss the long-term effects of the low-FODMAP diet on gut health to ensure we make well-informed decisions for our well-being.
To help us successfully implement a low-FODMAP diet, we'll share principles and practical tips for meal planning, shopping, and food preparation. We'll also address common challenges and offer guidance to ensure our success. Nutritional considerations, stool monitoring, and strategies for personalizing our FODMAP approach will be covered to further refine our diets.
For the foodies among us, we'll get creative with cooking and meal planning, providing low-FODMAP recipes and meal ideas from diverse cuisines. We'll also discuss strategies for navigating restaurant menus, social events, and travel, along with batch cooking, meal planning, and food storage tips for a sustainable low-FODMAP lifestyle.
Finally, we'll delve into seasonal low-FODMAP foods, the role of fibers and probiotics in gut health alongside FODMAP management, and compare the low-FODMAP diet with other gut health-focused dietary interventions and strategies.
As you can guess that it’s going to be a comprehensive guide and one email will be too short to encapsulate the details we want to share, so we will divide this into three parts series.
In this three-part series, we will cover the following topics:
Part 1: Foundations and Science
Foundations of FODMAPs
Defining FODMAPs and their categories
The role of FODMAPs in digestion, absorption, and gut microbiome health
Identifying high- and low-FODMAP foods
FODMAPs and Digestive Disorders
The Science Behind the Low-FODMAP Diet
Part 2: Implementation and Personalization
Implementing The Low-FODMAP Diet
Principles and implementation of the low-FODMAP diet and Phases of the low-FODMAP diet: Elimination, Reintroduction, and Personalization
Practical tips for meal planning, shopping, and food preparation
Addressing common challenges and ensuring success
Nutritional Considerations on a Low-FODMAP Diet
Beginners, Intermediate, and Advanced Strategies for Personalizing Our FODMAP Approach
Part 3: Cooking, Meal Planning, and Additional Strategies
Creative Cooking and Meal Planning for a Low-FODMAP Diet
Strategies for navigating restaurant menus, social events, and travel
Batch cooking, meal planning, and food storage tips for a sustainable low-FODMAP lifestyle
Seasonal low FODMAP food for spring, summer, fall, and winter in categories such as vegetables, grains, seeds, nuts, fruits
Choosing the right fibers and their role in gut health alongside FODMAP management
Choosing the right probiotics and their role in gut health alongside FODMAP management
Comparing and Combining the low-FODMAP diet with other gut health-focused dietary interventions and strategies
Together, we'll master the art and science of FODMAPs, empowering us to make the best choices for our gut health and overall well-being. Let's begin this journey to FODMAP mastery with Part 1, where we will lay the groundwork by defining FODMAPs, exploring their role in digestion, and examining the science behind the low-FODMAP diet.
Foundations of FODMAPs
It is essential for us to have a solid understanding of the foundations of FODMAPs. This includes defining FODMAPs and their categories, understanding their role in digestion, absorption, and gut microbiome health, as well as identifying high- and low-FODMAP foods.
Defining FODMAPs and their categories
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are a group of short-chain carbohydrates and sugar alcohols that are poorly absorbed in the small intestine. The main categories of FODMAPs are:
Oligosaccharides: These include fructans and galacto-oligosaccharides (GOS), found in foods like wheat, onions, garlic, and legumes.
Disaccharides: The primary disaccharide in this context is lactose, which is present in milk and dairy products.
Monosaccharides: Fructose is the main monosaccharide of concern, found in high concentrations in foods like honey, apples, and pears, as well as high-fructose corn syrup.
Polyols: These sugar alcohols include sorbitol and mannitol, commonly found in stone fruits, mushrooms, and some artificial sweeteners.
The role of FODMAPs in digestion, absorption, and gut microbiome health
FODMAPs play a crucial role in the digestive process due to their poor absorption in the small intestine. When these carbohydrates pass through the digestive tract, they can exert osmotic effects, drawing water into the intestines. This can contribute to diarrhea or loose stools in some individuals.
Additionally, as FODMAPs reach the large intestine, they become fermented by gut bacteria. While fermentation is a natural process, excessive fermentation of FODMAPs can lead to gas production, bloating, and abdominal discomfort. For some people, particularly those with functional gastrointestinal disorders like irritable bowel syndrome (IBS), FODMAPs can trigger or exacerbate symptoms.
We talked about fiber and fermented food for gut health. It's important to note that FODMAPs are not inherently harmful. In fact, they can have beneficial effects on the gut microbiome for many individuals. However, for those with FODMAP sensitivities, managing their intake can be key to maintaining gut health and minimizing symptoms.
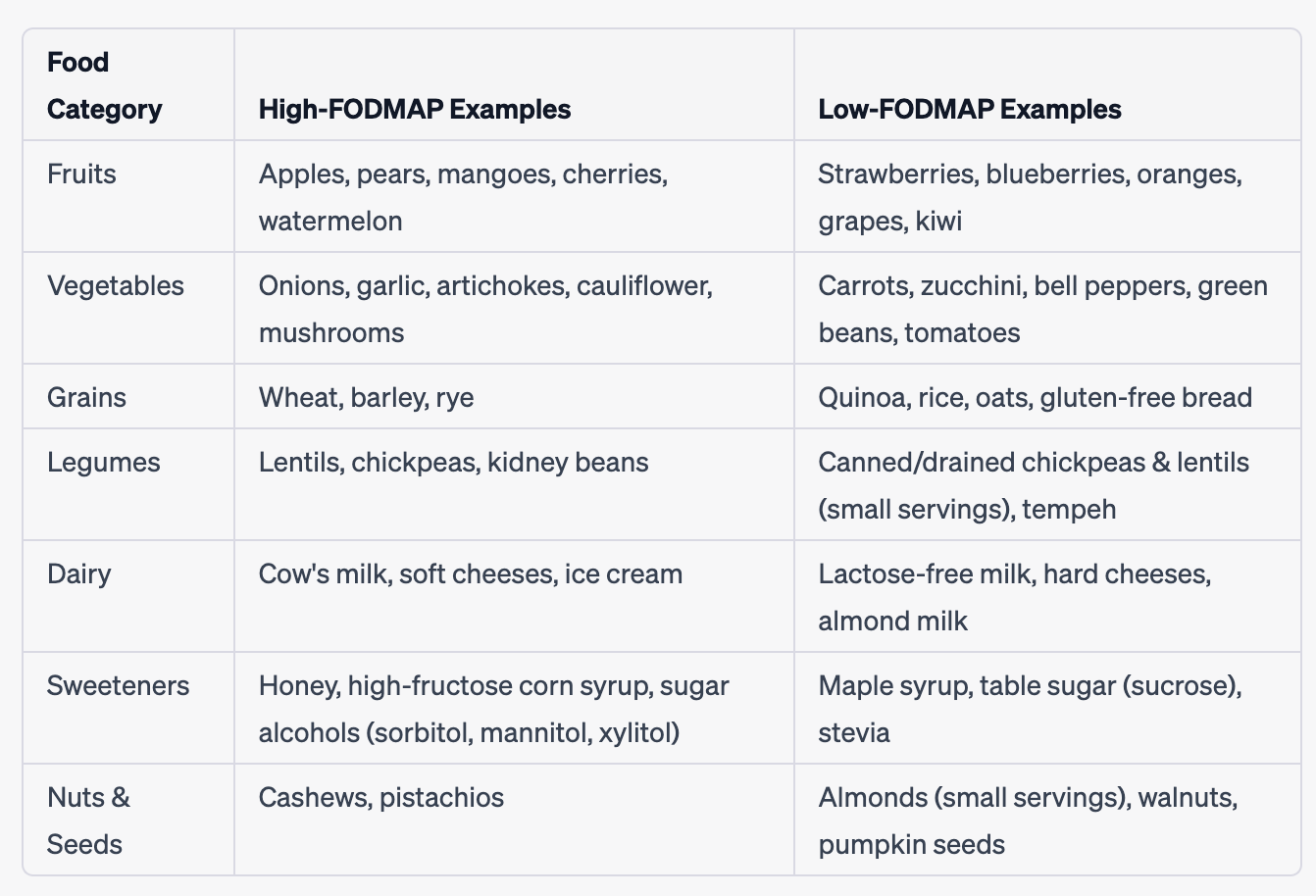
Identifying high- and low-FODMAP foods
Recognizing high-FODMAP foods and their low-FODMAP alternatives is crucial for managing FODMAP intake so that we can substitute high FODMAP fiber and fermented food with low FODMAP fiber and fermented food. Here are some examples of high- and low-FODMAP foods in various categories:
Fruits:
High-FODMAP: Apples, pears, mangoes, cherries, and watermelon
Low-FODMAP: Strawberries, blueberries, oranges, grapes, and kiwi
Vegetables:
High-FODMAP: Onions, garlic, artichokes, cauliflower, and mushrooms
Low-FODMAP: Carrots, zucchini, bell peppers, green beans, and tomatoes
Grains:
High-FODMAP: Wheat, barley, and rye
Low-FODMAP: Quinoa, rice, oats, and gluten-free bread
Legumes:
High-FODMAP: Lentils, chickpeas, and kidney beans
Low-FODMAP: Canned and drained chickpeas and lentils (in small servings), and tempeh
Dairy:
High-FODMAP: Cow's milk, soft cheeses, and ice cream
Low-FODMAP: Lactose-free milk, hard cheeses, and almond milk
Sweeteners
High-FODMAP: Honey, high-fructose corn syrup, and sugar alcohols (sorbitol, mannitol, xylitol)
Low-FODMAP: Maple syrup, table sugar (sucrose), and stevia
Nuts and Seeds:
High-FODMAP: Cashews and pistachios
Low-FODMAP: Almonds (in small servings), walnuts, and pumpkin seeds
Table below summarizes the high and low FODMAP food examples.
FODMAPs and Digestive Disorders
Most of us read this because we have one form or another form of digestive disorders. We already hinted above that high FODMAP food can exacerbate IBS symptoms. Let’s look into some more detail about FODMAPs and Digestive Disorders.
We will explore the role of FODMAPs in Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD), Small Intestinal Bacterial Overgrowth (SIBO), and other functional gastrointestinal disorders.
Irritable Bowel Syndrome (IBS):
IBS is a functional gastrointestinal disorder characterized by chronic abdominal pain, bloating, and alterations in bowel habits. Research has shown that for many individuals with IBS, a low-FODMAP diet can significantly improve symptoms. The reason is that FODMAPs can cause increased gas production and changes in intestinal motility, which can exacerbate IBS symptoms in some people. By reducing FODMAP intake, we can minimize the fermentation and osmotic effects that contribute to IBS symptoms, providing relief for many sufferers.
Inflammatory Bowel Disease (IBD):
IBD includes Crohn's disease and ulcerative colitis, both of which involve chronic inflammation in the digestive tract. While the low-FODMAP diet is not a primary treatment for IBD, some individuals with IBD may experience IBS-like symptoms or have concurrent IBS. In these cases, a low-FODMAP diet may help alleviate symptoms such as bloating, gas, and abdominal pain. It's essential to work closely with a healthcare professional when managing IBD, as the condition often requires a multifaceted treatment approach, including medication, lifestyle changes, and dietary modifications tailored to the individual's needs.
Small Intestinal Bacterial Overgrowth (SIBO):
SIBO occurs when there is an excessive amount of bacteria in the small intestine, leading to symptoms such as bloating, gas, diarrhea, and abdominal pain. While FODMAPs do not directly cause SIBO, they can contribute to symptoms in individuals with the condition. A low-FODMAP diet may help manage symptoms by reducing the substrate available for bacterial fermentation in the small intestine. However, it is important to note that a low-FODMAP diet is not a primary treatment for SIBO, and antibiotics or other treatments may be necessary to address the underlying bacterial overgrowth.
Other functional gastrointestinal disorders:
Other functional gastrointestinal disorders, such as functional dyspepsia or chronic idiopathic constipation, may also be influenced by FODMAP intake. While the evidence for the effectiveness of a low-FODMAP diet in these conditions is less robust than for IBS, some individuals may still benefit from reducing their FODMAP intake to manage symptoms. As with any dietary intervention, it's essential to work with a healthcare professional to develop a personalized approach that takes into account the individual's specific needs and circumstances.
It is clear that Low-FODMAP Diet can impact digestive disorders. Let’s understand the science behind the Low-FODMAP Diet.
The Science Behind the Low-FODMAP Diet
The low -FODMAP diet has gained popularity in recent years as a potential solution for individuals experiencing gastrointestinal discomfort and symptoms associated with Irritable Bowel Syndrome (IBS). We will explore the latest research, mechanisms of action, and the long-term effects of the low-FODMAP diet on gut health.
Latest research on the low-FODMAP diet's impact on gut health
Recent studies have demonstrated the effectiveness of the low-FODMAP diet in alleviating IBS symptoms in a significant proportion of patients. When we consume a diet high in FODMAPs, these carbohydrates can create an osmotic effect in the gut, leading to increased water retention, gas production, and abdominal discomfort.
Research has shown that a low-FODMAP diet can improve symptom control in up to 70-80% of people with IBS. These findings suggest that reducing the intake of FODMAPs can help manage gastrointestinal symptoms in many individuals.
Mechanisms of action: how FODMAPs influence gut microbiome and symptoms
The low-FODMAP diet works through a combination of mechanisms that influence the gut microbiome and alleviate symptoms. First, FODMAPs are osmotically active, which means they can draw water into the gut. When we reduce our FODMAP intake, there is less water retention in the intestine, leading to decreased bloating and abdominal discomfort.
Second, FODMAPs are rapidly fermented by gut bacteria, producing gas as a byproduct. A high-FODMAP diet can cause excessive gas production, leading to further bloating, pain, and altered bowel habits. By consuming a low-FODMAP diet, we can minimize this fermentation process and reduce gas production, thus alleviating these symptoms.
Moreover, recent research suggests that the low-FODMAP diet can lead to alterations in the gut microbiome composition. While the long-term implications of these changes are not yet fully understood, some studies have shown that a low-FODMAP diet can increase the abundance of beneficial bacterial species, potentially contributing to improved gut health.
The long-term effects of the low-FODMAP diet on gut health
It is important to consider the long-term effects of the low-FODMAP diet on gut health. While the diet has proven effective in managing IBS symptoms in the short term, the impact of prolonged adherence to the diet is less clear. Some concerns have been raised regarding potential negative effects on the gut microbiome, as the reduction of FODMAPs might also decrease the intake of certain prebiotic fibers that are essential for maintaining a healthy gut microbiome. These fibers serve as food for beneficial gut bacteria, promoting their growth and activity. We talked about Fiber extensively in one of our previous newsletters. Here is the link.
However, it's essential to note that the low-FODMAP diet is not meant to be a permanent solution. Instead, it should be viewed as a tool to help identify and manage individual triggers for IBS symptoms. After a period of strict adherence to the low-FODMAP diet, we recommend gradually reintroducing higher FODMAP foods to determine personal tolerance levels. This approach helps us identify specific food triggers while maintaining a diverse and balanced diet to support gut health in the long term.
Next
Now that we've explored the foundations and science of FODMAPs, we're better equipped to understand their impact on our gut health. However, this is just the beginning. In Part 2 of our FODMAP Mastery newsletter series, we'll delve into the practical side of things by discussing how to successfully implement and personalize the low-FODMAP diet. We'll cover everything from meal planning and shopping to addressing common challenges and ensuring success. Stay tuned for Part 2, where we'll provide the tools and strategies necessary for a seamless transition to a low-FODMAP lifestyle tailored to our unique needs. Don't miss it!
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
If you haven’t already subscribed then our sincere request, please subscribe.
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
gutsphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.