Repopulation, Recovery, and Responsible Use: Empowering Gut Microbiome After Antibiotics
Harnessing the Power of Pro-, Pre-, and Synbiotics: Navigating Success Signs and Heeding Help Signals in the Microbiome Revival Journey
Welcome Back Gutsphere Friends,
Welcome, my friend, to Part 6: Repopulation, Recovery, and Responsible Use. We've come a long way together, understanding the marvelous world of our gut microbiome, exploring the effects of antibiotics, and equipping ourselves with strategies to nurture our gut back to health. It's been a journey of discovery, hasn't it? But our expedition is far from over.
In this section, we're going to delve even deeper. Picture this: We've walked through the storm, braved the elements, and now we're on the other side. It's time for recovery and rebuilding. Our gut microbiome, just like a devastated city, needs help to repopulate and recover.
And guess what? We're not alone in this mission. We have powerful allies: probiotics, prebiotics, and synbiotics. These are not just fancy scientific terms; they're vital players in our gut ecosystem. They help us rebuild and maintain our gut health, acting as the architects and caretakers of our microbial city.
As we go forward, we'll be discussing how to recognize the signs of successful microbiome repopulation. And what about persisting symptoms or challenges? Don't worry, we've got that covered too. We'll learn when to seek help and what our next steps might be.
Research suggests that our gut microbiome, a complex ecosystem of trillions of bacteria, fungi, viruses, and other microorganisms, can begin to show signs of recovery around 1.5 months after the completion of an antibiotic course[1]. This timeline, however, is a generalized estimate. It's crucial to understand that the recovery of our gut microbiome post-antibiotics can be influenced by a variety of factors and can, therefore, differ significantly among individuals.
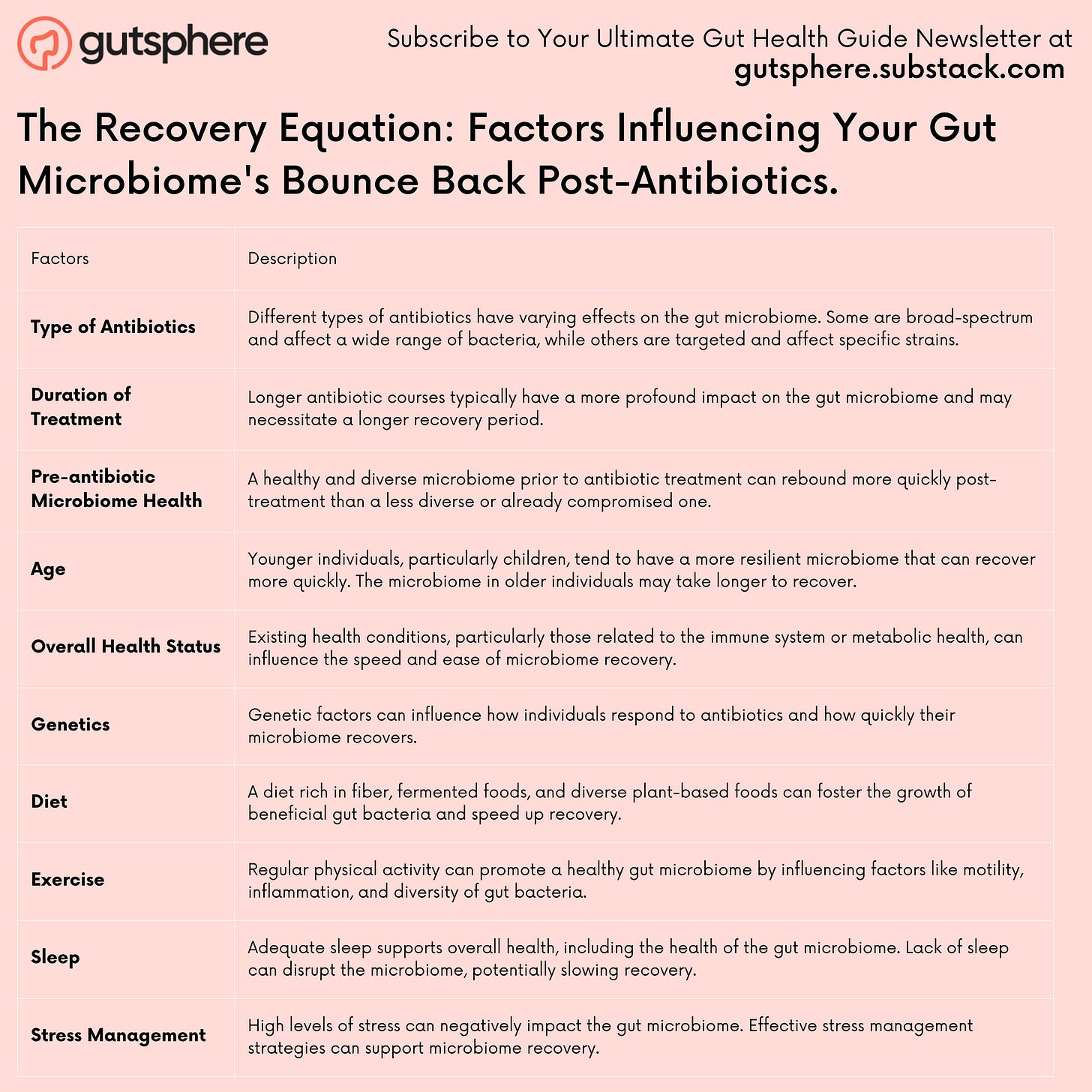
Several factors can influence this recovery timeframe. For instance, the specific types of antibiotics used, the duration of treatment, the initial health and diversity of your microbiome, your age, overall health status, and even genetics can all play a role in how quickly your gut microbiome can bounce back.
Furthermore, lifestyle factors like diet, exercise, sleep, and stress management can also impact the pace of recovery. A diet rich in diverse plant-based foods, fiber, and fermented foods can provide the necessary nutrients to foster the growth of beneficial gut bacteria. Regular exercise, adequate sleep, and effective stress management strategies can also support overall gut health and recovery post-antibiotics.
As such, it's essential to approach this recovery period with patience and perseverance. It might be tempting to seek quick fixes or feel frustrated if progress seems slow, but remember, restoring the gut microbiome is more like running a marathon than a sprint. It's a journey that requires consistent efforts in maintaining a healthy lifestyle and, when needed, working closely with healthcare providers to monitor progress and make necessary adjustments.
So, let's dive into Part 6. It's not just about recovery, it's about learning to use antibiotics responsibly, understanding our bodies better, and fostering a lifelong friendship with our gut microbiota. Ready for the next leg of our journey? Let's get started!
References:
The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4831151/
The Recovery Equation: Factors Influencing Your Gut Microbiome's Bounce Back Post-Antibiotics.
Here's a comprehensive table that outlines the various factors that can influence the recovery of the gut microbiome post-antibiotics:
Allies in Arms: Probiotics, Prebiotics, and Synbiotics in Our Journey of Gut Microbiome Recovery Post-Antibiotics
Sometimes, after we've weathered the storm of antibiotic therapy, our gut can feel a little like a war-torn landscape. But guess what? We're not alone in this fight. We have some fantastic allies waiting to march alongside us - probiotics, prebiotics, and synbiotics. They are ready to help us recover and repopulate our gut microbiome.
For now, we will give a brief overview on this. We plan to do a deep dive on probiotics, prebiotics, and Synbiotics in future.
Probiotics: Our Benevolent Bacteria Buddies
Probiotics are live microorganisms that, when ingested in adequate amounts, bestow health benefits upon us. They're like the cavalry coming in to assist in reestablishing the beneficial gut bacteria that the antibiotics might have marched over.
Research shows promise in the effectiveness of probiotics. For instance, a review published in the "Journal of Clinical Gastroenterology" indicated that certain strains of probiotics like Lactobacillus rhamnosus and Saccharomyces boulardii could prevent antibiotic-associated diarrhea.
But remember, probiotics are not one-size-fits-all. Their effectiveness can depend on factors like the strain of the probiotic, our unique gut microbiome, and our overall health. So, it's really worth chatting with our healthcare provider to select the probiotic best suited for us.
Furthermore, we have done a masterclass in fermented food which contains probiotics. Please check the link.
Prebiotics: The Gut Gardeners
While probiotics are like 'seeds', prebiotics are more like 'fertilizer' for our gut garden. They are non-digestible food components that promote the growth of beneficial bacteria in the gut, acting as their preferred food source. Inulin, fructo-oligosaccharides (FOS), and galacto-oligosaccharides (GOS) are common types of prebiotics.
Adding prebiotic-rich foods to our meals, think chicory root, garlic, onion, and whole grains, can provide some much-needed nourishment for our beneficial bacteria, aiding in the recovery of our gut microbiome.
Synbiotics: The Best of Both Worlds
Synbiotics are a combination of probiotics and prebiotics. They've been designed to ensure the survival and activity of the beneficial bacteria (probiotics) in our gut by providing them with their preferred food source (prebiotics). This combo can potentially enhance the efficacy of probiotics, promoting a more balanced gut microbiome.
Holistic Methods for Microbiome Recovery and Health
And it's not just about probiotics, prebiotics, and synbiotics. We need to consider our lifestyle as a whole if we want our gut microbiome to recover and thrive.
We have done masterclasses exercises and stress management. We can link it below. But here is a quick summary.
Regular Exercise: Regular physical activity has been linked to a more diverse and abundant population of beneficial gut bacteria. So, including moderate exercise in our daily routine can offer a significant boost to our gut health.
Adequate Sleep: Sleep and our gut health influence each other in a bidirectional way. Poor sleep can affect our gut microbiome, potentially leading to dysbiosis. So, it's essential to ensure we're getting around 7-9 hours of quality sleep each night.
Stress Management: Chronic stress can mess up the balance of our gut microbiome. Using stress management techniques such as mindfulness, yoga, or even just deep breathing exercises can help keep our stress levels (and our gut) in check.
We need to remember that our journey to recovery of our gut microbiome post-antibiotics is, well, a journey. It might be a slow process, but with patience, the right allies, and a balanced lifestyle, we can work towards a healthy and flourishing gut microbiome.
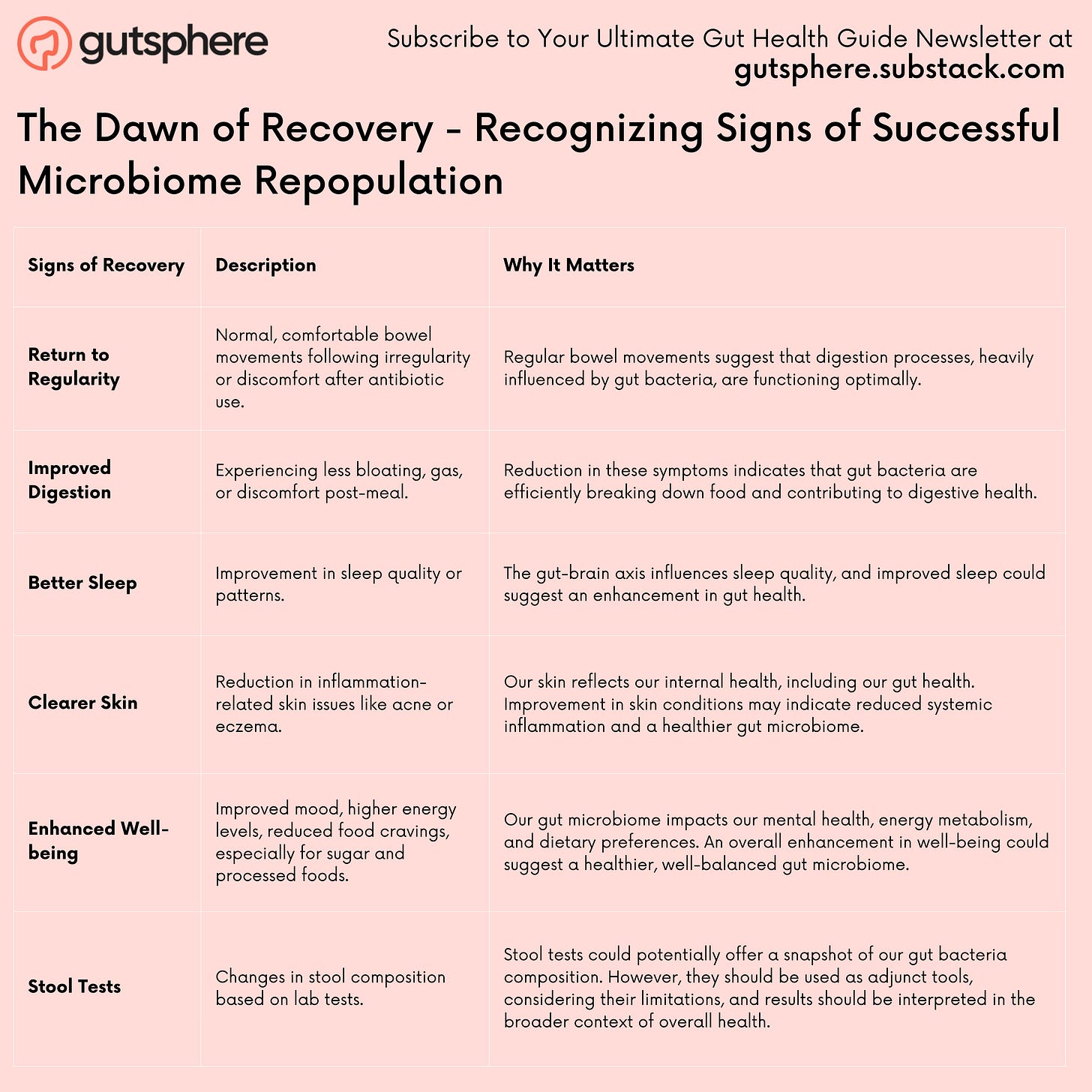
The Dawn of Recovery - Recognizing Signs of Successful Microbiome Repopulation
As we venture along the path of gut microbiome recovery following antibiotic use, it's natural to wonder when we've reached our destination. How do we know when our gut microbiome is back in balance? What signs should we look out for to indicate that our efforts in diet, lifestyle, and possibly supplemental interventions are bearing fruit? Let's explore some of these signals of successful microbiome repopulation.
Return to Regularity
One of the most apparent signs of gut microbiome recovery is a return to normal bowel movements. After an antibiotics course, if we've noticed changes like increased frequency, diarrhea, or irregularity, the easing of these symptoms can be a good indicator that our microbiome is bouncing back. Regular, comfortable bowel movements signify that our digestive processes, to which gut bacteria contribute significantly, are back on track.
Improved Digestion
Relatedly, improved digestion is another positive sign. Less bloating, gas, and discomfort post-meal can suggest that our gut bacteria are efficiently breaking down food and producing beneficial metabolites. Remember, our gut microbes play a crucial role in fermenting indigestible fibers and producing short-chain fatty acids (SCFAs), which not only aid in digestion but also have numerous health benefits.
Restful Sleep and Clearer Skin
It may surprise some of us, but the condition of our gut can influence the quality of our sleep and the health of our skin. Emerging research suggests a bidirectional relationship between gut health and sleep, with disruptions in one potentially affecting the other. Therefore, experiencing better sleep might suggest an improvement in our gut microbiome.
Similarly, our skin is a reflection of our internal health, including our gut. A decrease in inflammation-related skin issues like acne or eczema may suggest that our gut microbiome is stabilizing and reducing systemic inflammation.
General Sense of Well-being
Lastly, a general sense of well-being, both physically and mentally, is a powerful signal of gut microbiome recovery. This could manifest as improved mood, higher energy levels, or even lessened food cravings, especially for sugar and processed foods.
Stool Tests: A Tool with Limitations
Stool tests to analyze our gut bacteria composition could provide insights into microbiome recovery. However, it's essential to understand that this approach is not without its limitations. The gut microbiome is complex and dynamic, and while stool tests can offer a snapshot of our gut bacteria, they don't necessarily provide a comprehensive picture of our gut health. Furthermore, stool tests are just one piece of a larger puzzle that also includes our diet, lifestyle, genetics, and overall health. Nonetheless, they could potentially serve as an adjunct tool for monitoring changes and guiding dietary and lifestyle modifications.
Remember, our recovery journey after antibiotics use is deeply individual. The timeframe for seeing these signs can vary widely among us, influenced by various factors like the antibiotics used, the duration of treatment, our baseline gut health, and our diet and lifestyle. Most importantly, throughout this journey, patience and consistent efforts towards a healthier lifestyle are our best allies. Keep observing, adjusting, and listening to your body.
Persisting Symptoms and Seeking Professional Help: Navigating Post-Antibiotic Hurdles
Alright, we've done everything right, we've completed the antibiotic course as advised, followed a gut-friendly diet, embraced the probiotics and prebiotics, monitored our stool changes, and yet, something doesn't feel right. In fact, some of the symptoms seem to linger or, perhaps, even escalate. It's time we take a look at what might be happening and what our next steps should be.
Understanding Persisting Symptoms
Our body, in all its wisdom, has various ways of telling us when something isn't quite right. Persistent symptoms post-antibiotics can range from ongoing digestive issues, such as constipation, diarrhea, or bloating, to more systemic signs like fatigue, skin issues, and even mood disturbances. These could be signals that our gut microbiome is still in the recovery process, or it could mean that there's a deeper issue that needs to be addressed.
Recognizing When to Seek Help
So, when is the right time to seek help? If our symptoms persist for several weeks after we've finished our antibiotic course despite our best efforts at microbiome recovery, it may be time to get a healthcare provider involved. Another alarm bell should be if our symptoms significantly impact our day-to-day life or if we notice new, escalating, or concerning symptoms, such as high fever, severe abdominal pain, or blood in stool.
Possible Next Steps for Evaluation and Treatment
Further Testing: Depending on our symptoms and medical history, our healthcare provider might recommend further diagnostic tests. These could range from blood tests to check for any nutritional deficiencies or inflammation, stool tests to analyze the composition of our gut microbiota, or even an endoscopy or colonoscopy for a closer look at our gastrointestinal tract.
Dietary Modifications: Even if we're already on a gut-friendly diet, there might be some specific dietary changes our healthcare provider suggests based on our unique circumstances. For instance, they might recommend a low-FODMAP diet if we're dealing with persistent bloating and abdominal pain, or a gluten-free or dairy-free trial if they suspect food sensitivities.
Targeted Probiotic Therapy: While we might have already been taking a general probiotic, our healthcare provider might suggest a more targeted approach based on our specific needs. For instance, certain probiotic strains have been found particularly effective for conditions like antibiotic-associated diarrhea or irritable bowel syndrome.
Referral to a Specialist: If our symptoms are complex or if we're not responding to initial treatments, our healthcare provider might refer us to a gastroenterologist or another specialist. They can provide more advanced diagnostic and therapeutic options.
Remember, it's essential to listen to our bodies and seek professional help when needed. Every individual's journey with their gut health is unique, and sometimes, it takes a bit of trial and error to figure out what works best for us. Don't get disheartened by the bumps in the road, and remember, we're in it for the long haul towards optimal health.
The Fine Balance - Responsible Antibiotic Use for a Healthy Microbiome
We've ventured on a comprehensive journey exploring the intricate relationship between antibiotics and our gut microbiome. It's clear that antibiotics, while often lifesaving, can pose significant challenges to our gut health. But, it's not about eliminating antibiotics completely from our life - it's about achieving a fine balance.
Understanding Antibiotics: A Double-Edged Sword
Antibiotics are a valuable tool in our fight against harmful bacterial infections. Yet, they don't distinguish between the 'bad' bacteria causing our infections and the 'good' bacteria that support our health. Broad-spectrum antibiotics, in particular, can cause extensive disruption to our gut microbiome, leading to short-term and potentially long-term health issues.
Responsible Antibiotic Use
We have a significant role in fostering responsible antibiotic use. We should understand that antibiotics are not a cure-all. They're ineffective against viral infections like the common cold, the flu, and most sore throats. Taking antibiotics when they're not needed can lead to antibiotic resistance, a global health concern.
Here are some key guidelines for responsible antibiotic use:
Follow Prescriptions: Always take antibiotics exactly as prescribed by a healthcare provider. We should never skip doses or stop taking an antibiotic earlier than directed, even if we're feeling better.
No Self-Prescription: We should never use leftover antibiotics or take antibiotics prescribed for someone else. Each antibiotic regimen should be tailored to our specific infection and overall health condition.
Open Communication with Healthcare Providers: It's crucial that we discuss all our health concerns with our healthcare provider, including any problems we're experiencing with our gut health. They can help guide us through our treatment options and potential side effects.
Prevent Infections: One of the best ways to reduce our need for antibiotics is to stay healthy and prevent infections. This means getting regular exercise, eating a balanced diet, washing our hands regularly, and building immune system.
The Way Forward
As the field of microbiome research continues to evolve, we're learning more and more about how we can support our gut health in the face of necessary antibiotic use. And while science advances, it's also up to us to implement these findings in our lives and make informed decisions about our health.
Responsible antibiotic use coupled with focused efforts on maintaining and restoring gut health, creates a balanced and health-conscious approach. Remember, our gut health isn't just about how we're feeling right now, it's a critical aspect of our overall long-term health and wellbeing. It's an ongoing journey, but one well worth the effort
Series Conclusion: Triumph Over the Challenge - Mastering Your Gut Health Post-Antibiotics
What a journey we've embarked upon together! From understanding the deep and intricate connection between our gut microbiome and antibiotics, through exploring various recovery strategies, signs of successful repopulation, when to seek help and, lastly, the vital role of responsible antibiotic use, we've explored each turn and twist in the intricate labyrinth of our gut health.
The human body is an incredibly complex machine, with each part playing a critical role in maintaining overall health. Our gut microbiome is an essential piece of this intricate puzzle, and it's heartening to see the growing recognition of its importance.
Understanding how antibiotics affect our gut microbiome and the steps we can take to support recovery post-antibiotics empowers us to take an active role in our health. Armed with this knowledge, we can make informed decisions about antibiotic use, monitor our gut health, and seek help when needed.
While antibiotics are a necessary tool in our healthcare arsenal, we have also learned to appreciate their impact on our gut microbiome and to use them responsibly. Through balanced nutrition, probiotic supplementation, lifestyle modifications, and an open dialogue with our healthcare providers, we can help our gut microbiome recover and thrive after antibiotic use.
Looking Ahead: The Next Adventure - The Intersection of Sleep, Circadian Rhythm, and the Gut Microbiome
Just when we think we've unveiled all the secrets of our gut health, another exciting area of research beckons us. We've seen how our gut microbiome interacts with what we eat and the medications we take. But did you know that our sleep and circadian rhythms, the internal "body clock" that governs our sleep-wake cycle and physiological processes, are also intricately tied to our gut health?
As the sun sets on this series, a new day dawns on our next adventure where we dive into the fascinating world of sleep, circadian rhythms, and the gut microbiome. From the impacts of late-night snacking and sleep deprivation on our gut health, through the role of our gut microbiome in sleep quality, to how mastering our body clock can support a healthy microbiome - there's much to explore.
So, rest well, and gear up for our next enlightening journey through the interplay of sleep, circadian rhythm, and gut health. The adventure continues!
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
If you haven’t already subscribed then our sincere request, please subscribe.
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
GutSphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.