The Antibiotic Paradox: Navigating Your Microbiome's Battlefield
A Comprehensive Guide to Understanding Antibiotics, Your Gut Health, and Their Impact on Your Wellbeing
Welcome GutSphere Friends,
Welcome to our new series, The Antibiotic Paradox: Navigating Your Microbiome's Battlefield. This is more than just a series of newsletters about antibiotics and gut health. It's our collective journey of discovery, understanding, and ultimately empowerment. And it all starts with a deeply personal and transformative story - the story of our founder.
Imagine a 9-month-old baby, on the brink of life, battling severe diarrhea and infestations of intestinal worms. That baby grew into a frail child, continually weakened by infections and diseases. His companions were not toys or storybooks, but antibiotics, prescribed by doctors and sometimes, even by those who had no right to prescribe.
"Money weighs more than your body," his mother would often say with a chuckle, referring to the hefty amount spent on his medical bills. And yet, behind that humor, was an unnerving reality: his health was a constant uphill battle, one made more challenging by the very 'solutions' that were supposed to bring relief. His gut, his foundation, had been rattled by the repeated use of antibiotics.
However, our founder is no stranger to challenges, and his spirit remained undeterred. When his health issues subsided during his teenage years and he could finally distance himself from antibiotics, he thought it was a victory. But little did he know that his war was far from over. His disrupted microbiome haunted him with chronic constipation - a stark reminder of a battlefield that had never truly healed.
It's been a long, arduous journey since then, filled with curiosity, discovery, and quite a few surprises. He learned about the foundational role of the gut microbiome in health, and how the reckless use of antibiotics can devastate this delicate ecosystem. What shocked him even more was the increasing prevalence of antibiotics prescription worldwide, and the nonchalant attitude towards it in places like Nepal, where he grew up.
This experience has shaped his perspective on medication. He recognizes the power of antibiotics and appreciates their life-saving potential. But he also firmly believes that prevention should be our first line of defense and that intervention, although crucial at times, must be a carefully weighed decision. To him, medication, especially antibiotics, is not the enemy. It's the absence of careful judgment in using them that poses a risk.
This series is inspired by his personal quest - a quest that emerged from struggle and transformed into a beacon of knowledge for all of us. We're here to dig deep, uncover truths, and challenge long-held beliefs. We're here to guide you through the complexities of antibiotics, the subtleties of your gut microbiome, and the profound ways in which they intersect.
Our journey might be filled with paradoxes and conundrums, but remember, we're in this together. With every discovery we make, with every myth we bust, we become more capable of navigating the battlefield that is our gut. So, let's buckle up and embark on this quest - one that promises better health, empowered decisions, and a stronger foundation.
Here's to our health and our journey!
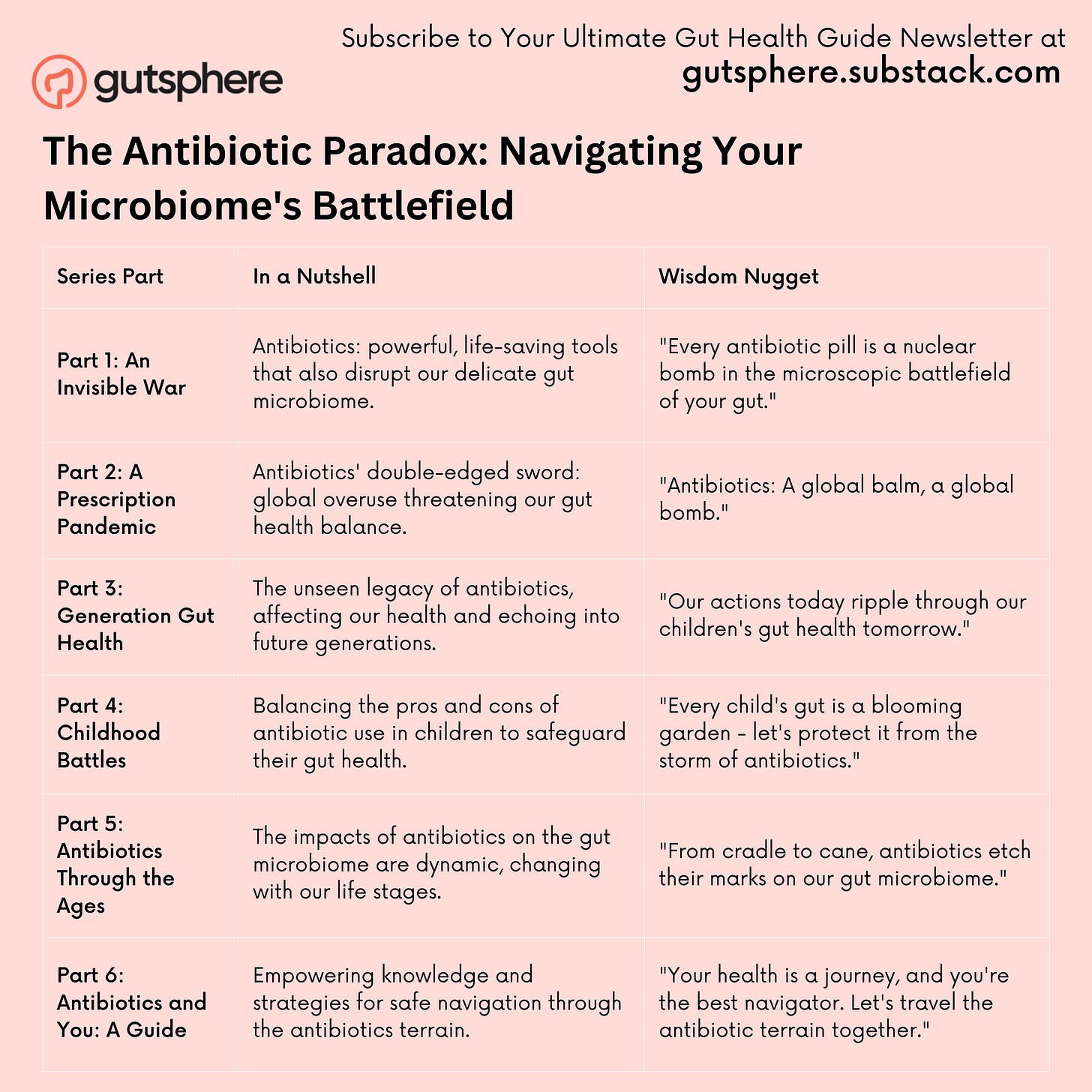
As we peel back the layers of this complex, fascinating topic over our six-part series, we'll delve into the following themes:
Part 1: The Invisible War: Antibiotics vs. Bacteria
Here, we'll explore the basics of antibiotics and their mechanisms of action against bacteria. It's like a tiny, microscopic war being waged inside your body, and understanding it is the first step to managing it.
Part 2: Too Much of a Good Thing: The Prevalence of Antibiotic Prescription
Antibiotics have become a household name, and in this part, we'll look at how widespread their use has become, and more importantly, whether that's a good thing.
Part 3: Our Shared Legacy: Inter-Generational Impact of Antibiotics & Childhood Antibiotic Use
Next, we'll look at how antibiotics affect us from the very earliest stages of our lives and how these impacts can echo across generations.
Part 4: Life Stages and Antibiotics: How Age Shapes Our Microbiome
This part dives into how antibiotics affect us differently at different stages of life, from infancy to old age, and how our microbiome evolves with us.
Part 5: Hidden Connections: Antibiotics and Diseases & Personalizing Your Approach to Antibiotics
It's time to connect the dots between antibiotics, diseases, and the gut microbiome. We'll uncover the web of connections and guide you on making informed decisions about antibiotics use.
Part 6: After the Storm: Monitoring and Restoring Your Gut Health Post-Antibiotics
Finally, we'll walk you through the process of rebuilding your gut's microbiome after a course of antibiotics. We'll provide practical tips and strategies for quickening microbiome recovery and spotting signs of successful repopulation.
So, buckle up, and let's set off on this enlightening journey together. Let's delve into the mystery that is our gut, understand the impact of antibiotics, and discover ways to restore and maintain a healthy gut microbiome. Here's to our collective wellbeing and a more informed approach to antibiotic use!
Below is the summary of the entire in a tabular format. It's a condensed version of the entire series, offering a brief overview of key points.
Before we go ahead in each of the series. Here is a bit more elaborated summary.
The Invisible Battle Within
Every time we take an antibiotic, a battle rages within us. This series aims to demystify the complex dynamics of antibiotics and our gut microbiome. We lay out the mechanisms of antibiotics, differentiating between various types and how each interacts uniquely with our internal ecosystem. From broad-spectrum antibiotics, akin to carpet bombing, to targeted antibiotics, which mirror a surgical strike, we come to understand why antibiotics are truly a double-edged sword.
The Double-Edged Sword
In this section, we grapple with the paradoxical nature of antibiotics. The use of antibiotics globally surged by 65% between 2000 and 2015. We examine the worldwide differences in antibiotic usage and underline the potential risks of unregulated access in some countries. Additionally, we discuss the impact of antibiotics on the diversity and function of our gut microbiome, focusing on the rise of antibiotic-resistant bacteria, recognized as a global health challenge.
Legacy of Our Choices
The antibiotics we consume have an impact that extends beyond us; they leave a legacy. New research suggests that our use of antibiotics might influence our descendants' health. A link has been discovered between antibiotic exposure in early life and disease manifestation later in life. The concept of health effects being passed from parents to offspring, known as transgenerational effects, is central to this section.
Risks vs. Benefits in Childhood
Children are often the primary recipients of antibiotics. It's estimated that by the age of 20, the average American child will have received 17 courses of antibiotics. This part explores the potential long-term impacts of antibiotics on children's gut microbiota, the implications for their future health, and how parents can balance the immediate benefits against possible long-term effects.
Antibiotics Through Life's Stages
The influence of antibiotics isn't uniform for everyone. As we age, our gut microbiome evolves, altering the way antibiotics affect it. There's potential for different impacts based on life stages. We deeply investigate how age and life stage can significantly affect antibiotic impact on gut health, exploring the intricacies of each life stage.
Deciphering the Disease Links
Our comprehension of the gut-brain axis and the gut's role in overall health has significantly increased in recent years. Connections between antibiotic use and various diseases have started to appear. For example, one study linked antibiotic use in childhood to obesity later in life. However, it's crucial to remember that correlation doesn't imply causation. We delve into these links and unpack the subtleties.
Navigating the Antibiotics Dilemma
Decisions about antibiotic use can be perplexing. In this chapter, we present insights based on evidence to guide individuals in their dialogues with healthcare providers. We discuss the trade-off between the immediate benefits of antibiotics and potential long-term impacts on gut health. Evidence reveals that patients appreciate shared decision-making regarding antibiotic use, enabling us to actively participate in our health journeys.
Rescuing Your Gut Post-Antibiotics
Just as a forest can regrow after a wildfire, our gut can recover from an antibiotic onslaught. We look at what recovery entails and offer practical strategies to aid the process. Research shows that the gut microbiome can begin to recover within days but may take months or longer to return to its original state.
Spotting an Imbalance
Our bodies have an incredible ability to communicate if we learn to listen. This chapter helps readers comprehend potential signs of a gut microbiome imbalance following antibiotic use. Some symptoms like bloating or changes in bowel movements might be noticeable, while others like mood shifts or sleep disturbances could be subtler.
The Long Road to Recovery
Gut microbiome recovery isn't a quick process; it's a prolonged journey. We explore the timeframe for microbiome recovery post-antibiotics, explaining why the recovery period can vary greatly between individuals. Research has found that gut diversity might not fully recover until after six months post-antibiotics.
Allies in Recovery: Probiotics, Prebiotics, and Synbiotics
In the journey of gut health recovery, probiotics, prebiotics, and synbiotics can be our allies. We bring forward the latest research that reveals the potential benefits and limitations of these supplements in supporting gut microbiome recovery after antibiotics.
Beyond the Gut: A Holistic Approach
Our gut health doesn't exist in isolation. We discuss how maintaining a healthy lifestyle - regular exercise, adequate sleep, and stress management - can support gut health. A holistic approach can aid us in building resilience and better health.
Recognizing Success and Seeking Help
Success isn't always a straight line, and neither is gut microbiome recovery. We discuss potential signs of successful recovery, the role of stool tests, and when to consult a healthcare provider. Research highlights the potential for personalized gut health monitoring, while also noting the limitations of current methods.
The Future of Antibiotics: Precision Medicine
Our final chapter takes us into the future, where antibiotic use could become more targeted, reducing their impact on our gut microbiota. The concept of 'precision antibiotics' is under development, which could significantly alter our approach to bacterial infections and gut health.
References
The Invisible Battle Within:
"Action and resistance mechanisms of antibiotics: A guide for clinicians" , https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5672523/
The Double-Edged Sword:
Global increases in antibiotic consumption: a concerning trend for WHO targets., https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30456-4/fulltext
Legacy of Our Choices:
Intestinal microbiome is related to lifetime antibiotic use in Finnish pre-school children". https://www.nature.com/articles/ncomms10410
Long-Term Effects of Early-Life Antibiotic Exposure on Resistance to Subsequent Bacterial Infection, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6935859/
Risks vs. Benefits in Childhood:
Effects of early-life antibiotics on the developing infant gut microbiome and resistome: a randomized trial, https://www.nature.com/articles/s41467-022-28525-z
Impact of antibiotics on off-target infant gut microbiota and resistance genes in cohort studies, https://www.nature.com/articles/s41390-022-02104-w
Less is more: Antibiotics at the beginning of life, https://www.nature.com/articles/s41467-023-38156-7
Antibiotics Through Life's Stages:
Population-level impacts of antibiotic usage on the human gut microbiome. https://www.nature.com/articles/s41467-023-36633-7
The Gut Microbiome, Aging, and Longevity: A Systematic Review, https://pubmed.ncbi.nlm.nih.gov/33297486/
The gut microbiome as a modulator of healthy ageing, https://www.nature.com/articles/s41575-022-00605-x
The Gut Microbiota and Healthy Aging: A Mini-Review, https://pubmed.ncbi.nlm.nih.gov/30025401/
Deciphering the Disease Links:
"Antibiotics in early life alter the gut microbiome and increase disease incidence in a spontaneous mouse model of autoimmune insulin-dependent diabetes." PLOS ONE, 2015. Link
Navigating the Antibiotics Dilemma:
"Exploring patients’ attitudes towards antibiotic use for respiratory tract infections: a qualitative study in the context of a cluster-randomized controlled trial." The Journal of Antimicrobial Chemotherapy, 2020. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0125448
Rescuing Your Gut Post-Antibiotics:
Recovery of the Gut Microbiota after Antibiotics, Depends on Host Diet, Community Context, and Environmental Reservoirs, Cell, https://www.cell.com/cell-host-microbe/pdfExtended/S1931-3128(19)30535-9
Spotting an Imbalance:
"Gut microbiota in autism and mood disorders." https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698498/
The Long Road to Recovery:
Recovery of gut microbiota of healthy adults following antibiotic exposure, https://www.nature.com/articles/s41564-018-0257-9
Allies in Recovery: Probiotics, Prebiotics, and Synbiotics:
"Probiotics, prebiotics, and synbiotics: implications for human health." https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5622781/
Beyond the Gut: A Holistic Approach:
Microbiota in health and diseases, https://www.nature.com/articles/s41392-022-00974-4
Recognizing Success and Seeking Help
Gut Microbiome: Profound Implications for Diet and Disease, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6682904/
The Future of Antibiotics: Precision Medicine
Precision antimicrobial therapeutics: the path of least resistance?, https://www.nature.com/articles/s41522-018-0048-3
Next
Now that we've covered the broad strokes of what's to come, we hope you're as excited as we are to delve deeper into this fascinating and vital topic. As we prepare to embark on this complex journey, we'll equip you with the knowledge you need to understand the invisible battle that rages within us each time we take an antibiotic.
Next time, we're launching straight into Part 1: "The Invisible Battle Within," where we'll unravel the intricate dynamics of antibiotics and our gut microbiome. From the carpet-bombing tactics of broad-spectrum antibiotics to the surgical strikes of targeted ones, we'll explore how these powerful tools of modern medicine interact with the ecosystem within us. Stay tuned!
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
If you haven’t already subscribed then our sincere request, please subscribe
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
Gutsphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.