The Hemorrhoid Healing Masterclass: Conquer Hemorrhoids with Gut Health and Holistic Strategies(Part 1/4)
A Comprehensive Guide Uniting Modern and Traditional Medicine, Gut Microbiome Insights, and Lifestyle Changes for Lasting Relief
Welcome Back, Gutsphere friends!
Welcome to our comprehensive edition, where we'll embark on a journey to unravel the mysteries of hemorrhoids and arm ourselves with knowledge, practical strategies, and self-care techniques. Our goal is to empower you to tackle hemorrhoids with confidence and perseverance.
In this action-packed newsletter, we've divided the content into four engaging parts, each shedding light on various aspects of hemorrhoids, their management, and prevention.
🔍 Part 1: Understanding Hemorrhoids Get ready to dive deep into the world of hemorrhoids, where we'll explore their history, different stages, and causes. We'll also examine the critical role of the gut microbiome in hemorrhoid management.
💪 Part 2: Lifestyle and Self-Care Strategies Discover a holistic approach to hemorrhoid prevention and management, focusing on nutrition, exercise, stress management, and bathroom etiquette. We'll share valuable tips on embracing healthy habits that can make a significant difference in your hemorrhoid journey.
🌿 Part 3: Holistic and Traditional Treatment Approaches Learn about various holistic and traditional treatment methods, from Ayurveda and Traditional Chinese Medicine to modern medicine. We'll also delve into the realm of home remedies, oils, and surgical options, with an emphasis on understanding their benefits, risks, and side effects.
🎯 Part 4: Developing a Personalized Hemorrhoid Management Plan Master the art of creating a personalized hemorrhoid management plan by identifying triggers, monitoring progress, and recalibrating your approach. We'll also share practical advice from those who've successfully managed their hemorrhoids.
As we navigate through these four enlightening parts, we'll be uncovering everything you need to know about hemorrhoids, from understanding their intricacies to effective management and prevention strategies. So, buckle up and get ready to embark on this empowering journey towards a healthier, happier life free from the discomfort of hemorrhoids.
And stay tuned for our upcoming installment, where we'll tackle the often overlooked but crucial topic of constipation and its impact on hemorrhoids. Get ready to dive even deeper into the world of gut health and digestive well-being!
Part 1: Understanding Hemorrhoids: Causes, Symptoms, and Stages
We are very curious about the history of hemorrhoids. So, let’s begin with a brief history.
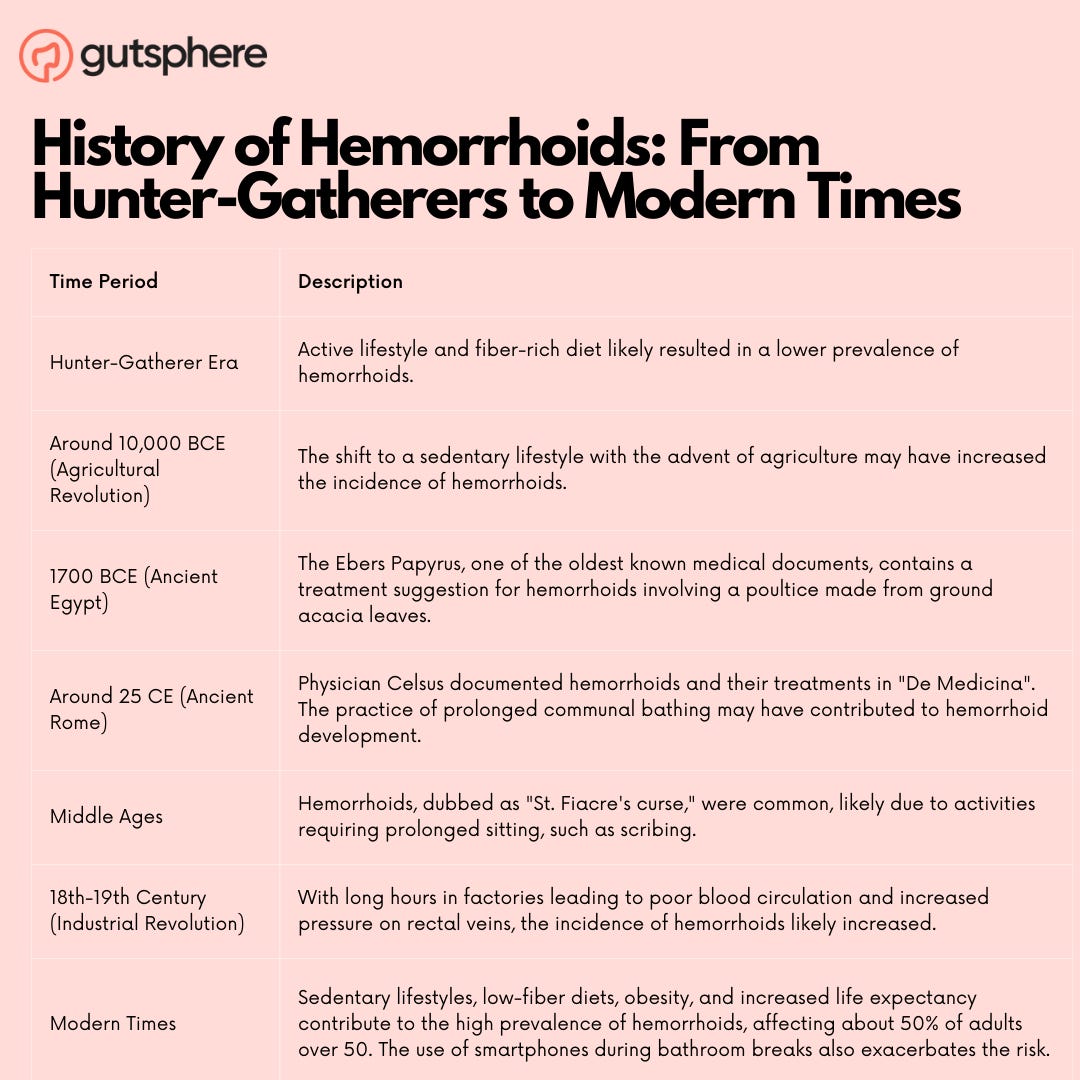
History of Hemorrhoids: "From Hunter-Gatherers to Modern Times: The Evolution of Hemorrhoids"
Hemorrhoids, the pesky, painful, and all-too-common ailment, have plagued humans for centuries. As we embark on this fascinating journey through time, let's explore the evolution of hemorrhoids, the first cases, and whether our hunter-gatherer ancestors experienced the same discomfort. Along the way, we'll discover how the significant lifestyle changes throughout human history have impacted the prevalence of hemorrhoids.
Our journey begins in the earliest chapters of human history. The first recorded mention of hemorrhoids dates back to ancient Egypt around 1700 BCE, where they were described in the famous Ebers Papyrus, one of the oldest known medical documents. The papyrus suggests that the Egyptians were aware of hemorrhoids and even recommended a treatment involving a poultice made from ground acacia leaves.
But what about our hunter-gatherer ancestors? Did they suffer from hemorrhoids as well? It's difficult to say for certain, but it's likely that they did, albeit at a much lower prevalence rate. Hemorrhoids are essentially swollen and inflamed veins in the rectal and anal region, which can be caused or exacerbated by factors such as constipation, straining during bowel movements, and prolonged sitting. Our hunter-gatherer ancestors led active lifestyles, which helped promote regular bowel movements and healthy blood circulation. Their diet, rich in fiber from fruits, vegetables, and nuts, would have contributed to healthy digestion and reduced the likelihood of constipation.
As human societies shifted from hunter-gatherer lifestyles to agriculture-based civilizations, our daily routines began to change significantly. With the advent of agriculture around 10,000 BCE, humans gradually transitioned to more sedentary lifestyles, spending long hours sitting or squatting while tending to their crops. This shift in physical activity may have led to an increased incidence of hemorrhoids in these early agricultural communities.
The story continues in ancient Rome, where the great Roman physician Celsus documented hemorrhoids and their treatment methods in his medical encyclopedia "De Medicina" around 25 CE. Romans, like many ancient civilizations, had adopted the practice of communal bathing, which involved sitting for extended periods in hot baths. This prolonged exposure to heat and moisture may have contributed to the development of hemorrhoids among the Roman population.
Fast forward to the Middle Ages, and we find that hemorrhoids were so common that they were given a nickname – "St. Fiacre's curse." St. Fiacre, the patron saint of hemorrhoid sufferers, was a 7th-century Irish monk who reportedly cured himself of hemorrhoids by sitting on a stone. This connection between hemorrhoids and sitting was becoming increasingly clear, as more and more people in various civilizations engaged in activities that required prolonged sitting, such as scribing or working on looms.
The Industrial Revolution, spanning the 18th and 19th centuries, brought about dramatic changes in human lifestyles, leading to further increases in hemorrhoid prevalence. As more people moved to urban areas and began working in factories, they spent long hours sitting or standing in one place, which contributed to poor blood circulation and increased pressure on the veins in the rectal area.
Today, hemorrhoids are estimated to affect approximately 50% of adults over the age of 50 in Western countries. Several factors contribute to the increased prevalence of hemorrhoids in modern populations, including sedentary lifestyles, low-fiber diets, obesity, and increased life expectancy. The use of smartphones and other electronic devices during bathroom breaks has also been shown to contribute to prolonged sitting and increased straining, exacerbating the risk of hemorrhoid development.
Despite the challenges presented by our modern lifestyles, we can learn valuable lessons from our ancestors. By looking back in time, we can recognize the importance of physical activity, proper posture, and a fiber-rich diet in preventing and managing hemorrhoids. In doing so, we can take control of our own health and wellbeing, just as our ancestors did.
While we can't reverse the clock and return to our hunter-gatherer roots, we can make conscious choices to improve our gut health and reduce the risk of developing hemorrhoids. Integrating daily exercise, even in the form of short walks or stretching breaks, can make a significant difference. By prioritizing movement, we promote healthy blood circulation and counteract the negative effects of our sedentary lifestyles.
In addition to exercise, we can also learn from the dietary habits of our ancestors. Consuming a diet rich in fruits, vegetables, whole grains, and legumes provides us with the fiber necessary for healthy digestion and regular bowel movements. By avoiding processed and low-fiber foods, we can minimize the risk of constipation and straining, two factors that contribute to hemorrhoid development.
Another crucial aspect of hemorrhoid prevention is proper bathroom habits. In many traditional cultures, squatting was the preferred position for bowel movements. This position helps to straighten the rectum and facilitate smoother elimination, reducing the need to strain. While it may not be practical to squat in every bathroom situation, we can adopt simple changes like using a footstool to elevate our feet, mimicking a squatting position and encouraging better bowel movements.
By examining the historical context of hemorrhoids, we can gain a deeper understanding of how our ancestors navigated this common ailment and learn valuable lessons for our own hemorrhoid management. By incorporating aspects of their active lifestyles and dietary habits, we can take meaningful steps towards preventing and treating hemorrhoids in the modern world.
In conclusion, tracing the history of hemorrhoids from hunter-gatherer societies to the present day has provided us with unique insights into the factors that have contributed to their increased prevalence over time. As we continue to navigate our modern lifestyles, it's essential to remember the lessons learned from our ancestors and prioritize gut health, physical activity, and proper bathroom habits to effectively prevent and manage hemorrhoids. Together, we can work towards a future where hemorrhoids are a relic of the past, rather than an ever-present concern.
That’s why we focus on increasing awareness and education, holistic self care. Let’s understand in detail.
Understanding the Different Stages of Hemorrhoids: "Hemorrhoids Demystified: Recognizing the Stages"
Hemorrhoids, the often misunderstood and stigmatized condition, affect millions of people worldwide. In fact, it is estimated that about 50% of adults will experience hemorrhoids by the age of 50. Despite their prevalence, many individuals are unaware of the different stages and when to seek professional help. We aim to demystify hemorrhoids, helping everyone recognize the stages, signs to watch for, and when to seek medical attention.
Understanding the Different Stages of Hemorrhoids
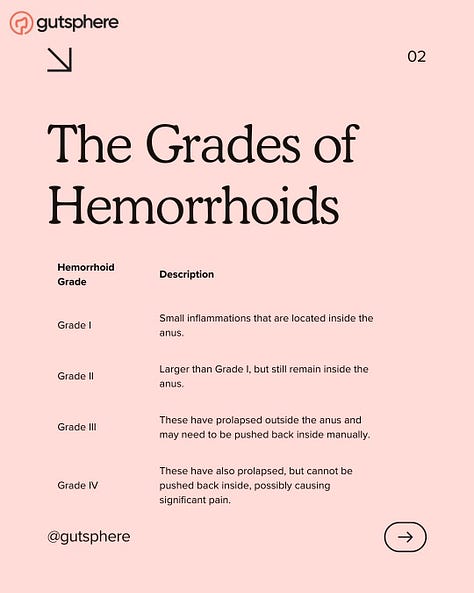
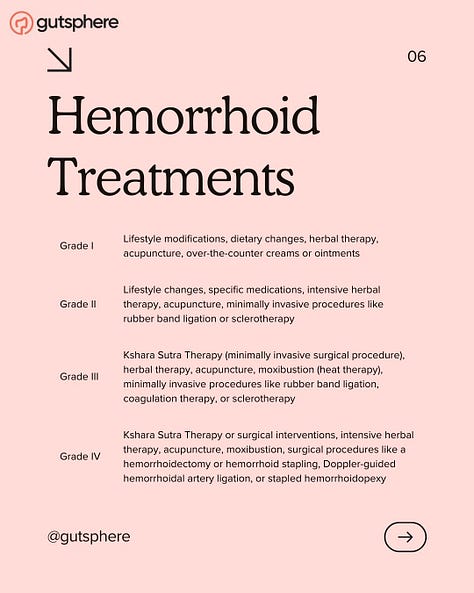
Hemorrhoids are swollen and inflamed veins in the rectal and anal area, which can be classified into four distinct stages:
Stage I: This initial stage is characterized by mild discomfort and small hemorrhoids that are not prolapsed (protruding from the anus). At this stage, hemorrhoids often cause itching, irritation, and occasional bleeding during bowel movements. However, these symptoms may go unnoticed by many individuals.
Stage II: As hemorrhoids progress to stage II, they begin to prolapse during bowel movements but retract on their own afterward. This stage is marked by increased discomfort, pain, and more frequent bleeding. The risk of complications, such as thrombosis (clotting), begins to rise at this stage.
Stage III: At this stage, hemorrhoids prolapse during bowel movements and may not retract on their own, requiring manual reinsertion. Symptoms become more severe, and individuals may experience a constant sensation of fullness, difficulty with hygiene, and increased pain.
Stage IV: The most advanced stage, stage IV hemorrhoids are permanently prolapsed and cannot be manually reinserted. Severe pain, bleeding, and complications such as strangulation (cutting off blood flow) and thrombosis are common. This stage often requires surgical intervention for relief.
Knowing When to Seek Professional Help
While hemorrhoids are common, it's essential to recognize when to consult a healthcare professional. The following are signs that it's time to visit a doctor:
Persistent bleeding: Occasional bleeding is not uncommon with hemorrhoids, but if we notice persistent or heavy bleeding, it's essential to consult a doctor. This may indicate a more severe issue, such as an anal fissure, colorectal polyps, or even colorectal cancer.
Severe pain: Although mild discomfort is typical with hemorrhoids, severe pain may indicate complications like thrombosis or strangulation. Immediate medical attention is necessary to avoid further complications.
Inability to manually reinsert prolapsed hemorrhoids: If we have stage III hemorrhoids and cannot reinsert them manually, it's important to consult a doctor. Prolonged prolapse can lead to strangulation and tissue death, requiring emergency treatment.
No improvement with at-home treatments: If our symptoms do not improve with over-the-counter remedies, lifestyle changes, or home treatments after 7 to 10 days, it's time to seek professional help. A healthcare provider can recommend more effective treatments or identify any underlying conditions contributing to your symptoms.
Pain, Effort, Color, and Quantity of Blood: What to Watch For
Monitoring our symptoms is crucial in identifying the stage of your hemorrhoids and determining whether to seek medical attention. Pay attention to the following signs:
Pain: While mild discomfort is common in the early stages, severe pain may indicate advanced hemorrhoids or complications. Take note of the intensity, duration, and triggers of your pain.
Effort: Are you straining excessively during bowel movements? Straining can worsen hemorrhoids and lead to complications. Adopting healthy bathroom habits, such as not forcing bowel movements and avoiding spending excessive time on the toilet, can help alleviate symptoms and prevent the progression of hemorrhoids.
Color: The color of the blood in your stool or on toilet paper can provide valuable information. Bright red blood typically indicates bleeding from hemorrhoids or an anal fissure, while darker blood may suggest bleeding from higher up in the digestive tract, which requires immediate medical attention.
Quantity of blood: While occasional spotting is not uncommon with hemorrhoids, consistently heavy bleeding or passing large blood clots warrants a visit to the doctor. Heavy bleeding could lead to anemia or indicate a more serious underlying issue.
Complications and When to Seek Immediate Medical Attention
Hemorrhoids, if left untreated or not managed properly, can lead to complications that require immediate medical attention. Some of the complications include:
Thrombosed hemorrhoids: When a blood clot forms within an external hemorrhoid, it is called a thrombosed hemorrhoid. This condition can cause severe pain, inflammation, and swelling. Thrombosed hemorrhoids may require surgical intervention to remove the clot and alleviate symptoms.
Strangulated hemorrhoids: In severe cases, prolapsed hemorrhoids may become strangulated, cutting off blood flow to the affected tissue. This can lead to tissue death (gangrene) and requires emergency treatment.
Anemia: Chronic blood loss from hemorrhoids can result in anemia, a condition characterized by a lack of red blood cells or hemoglobin in the blood. Symptoms of anemia include fatigue, shortness of breath, and pale skin. If you suspect anemia, consult your doctor immediately.
In conclusion, understanding the different stages of hemorrhoids, recognizing when to seek professional help, and monitoring your symptoms are crucial steps in managing this common condition. By staying informed and taking action, we can empower ourselves to prevent, treat, and conquer hemorrhoids. Remember that early intervention and adopting a proactive approach to your health can make all the difference in preventing complications and improving your quality of life.
Let’s understand what causes, risks factors contributing to the different stages of Hemorrhoids.
Causes and Risks Factors Contributing to Hemorrhoids: "The Roots of Hemorrhoids: Common and Uncommon Causes"
Hemorrhoids, also known as piles, are a common health issue that affects millions of people worldwide. While they can be uncomfortable and even painful, understanding their causes and risk factors can help us prevent and manage this condition effectively. We will dive into the common and uncommon causes of hemorrhoids, dispel some myths and misconceptions, and explore controllable and uncontrollable risk factors.
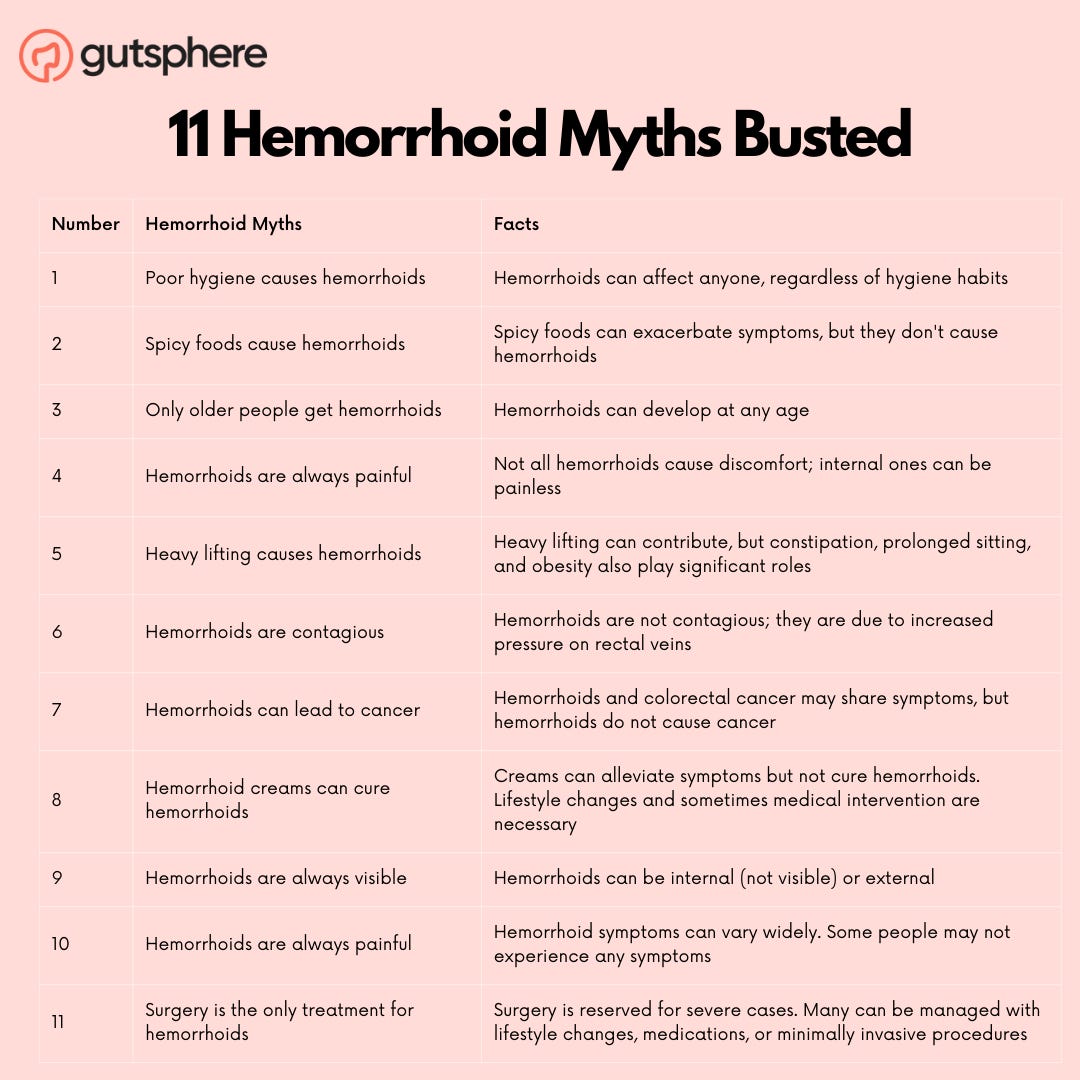
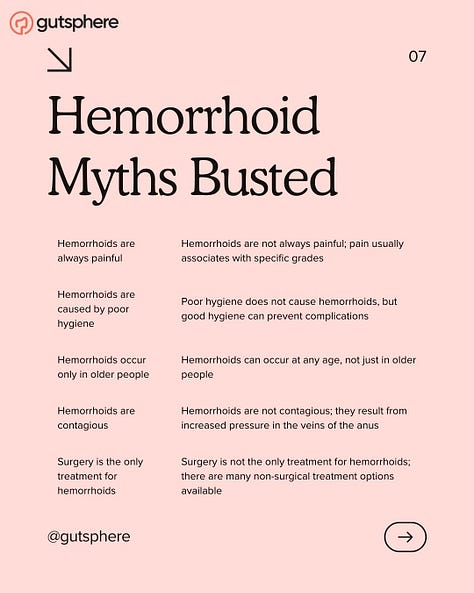
Myths and Misconceptions of Hemorrhoids
Before delving into the causes and risk factors, it's important to address some common myths and misconceptions surrounding hemorrhoids.
Myth 1: Hemorrhoids are a sign of poor hygiene.
Fact: Hemorrhoids can affect anyone, regardless of their hygiene habits. Maintaining good hygiene can help prevent infections and ease symptoms, but it will not prevent hemorrhoids from developing.
Myth 2: Hemorrhoids are caused by spicy foods.
Fact: While spicy foods can cause discomfort or exacerbate symptoms for some individuals, they do not directly cause hemorrhoids.
Myth 3: Only older people get hemorrhoids.
Fact: While the risk of developing hemorrhoids increases with age, young adults and even children can develop them as well.
Myth 4: Hemorrhoids are always painful.
Fact: While hemorrhoids can be painful, not all of them cause discomfort. Some individuals may have hemorrhoids without experiencing any pain or even being aware of their presence. Internal hemorrhoids, in particular, are often painless. However, if an internal hemorrhoid prolapses or becomes thrombosed (forms a blood clot), it can cause pain.
Myth 5: Hemorrhoids are a result of heavy lifting.
Fact: While heavy lifting and straining can contribute to hemorrhoid development in some cases, it is not the sole cause. Factors such as constipation, prolonged sitting, and obesity can also play a significant role in the development of hemorrhoids. If we’re concerned about heavy lifting causing hemorrhoids, consider using proper lifting techniques and engaging in regular exercise to strengthen our core muscles.
Myth 6: Hemorrhoids are contagious.
Fact: Hemorrhoids are not contagious and cannot be spread through contact with an affected individual. They are caused by increased pressure on the veins in the rectum and anus, which can be attributed to various factors such as straining during bowel movements, constipation, and obesity.
Myth 7: Hemorrhoids can lead to cancer.
Fact: While hemorrhoids and colorectal cancer may share some symptoms, such as rectal bleeding, hemorrhoids themselves do not cause cancer. However, if we experience persistent rectal bleeding, it's essential to consult a healthcare professional to rule out other potential causes, including cancer.
Myth 8: Hemorrhoid creams can cure hemorrhoids.
Fact: Hemorrhoid creams and ointments can help alleviate symptoms such as itching, swelling, and pain, but they do not provide a permanent cure for hemorrhoids. Lifestyle changes, such as adopting a high-fiber diet and engaging in regular exercise, are crucial for managing and preventing hemorrhoids long-term. In some cases, medical intervention may be necessary to treat persistent or severe hemorrhoids.
Myth 9:Hemorrhoids are always visible.
Hemorrhoids can be internal, external, or a combination of both. Internal hemorrhoids are located inside the rectum and may not be visible, while external hemorrhoids are visible and located outside the anus.
Myth 10: Hemorrhoids are always painful.
While hemorrhoids can cause discomfort, pain, and itching, some people may not experience any symptoms at all. The severity of hemorrhoid symptoms can vary widely depending on the individual and the underlying causes.
Myth 11: Surgery is the only way to treat hemorrhoids.
Surgery is typically reserved for severe or persistent cases of hemorrhoids that do not respond to more conservative treatments. Many cases of hemorrhoids can be effectively managed with lifestyle changes, over-the-counter medications, or minimally invasive procedures.
Common and Uncommon Causes
There are several common and uncommon causes of hemorrhoids, which we will explore below.
Common causes:
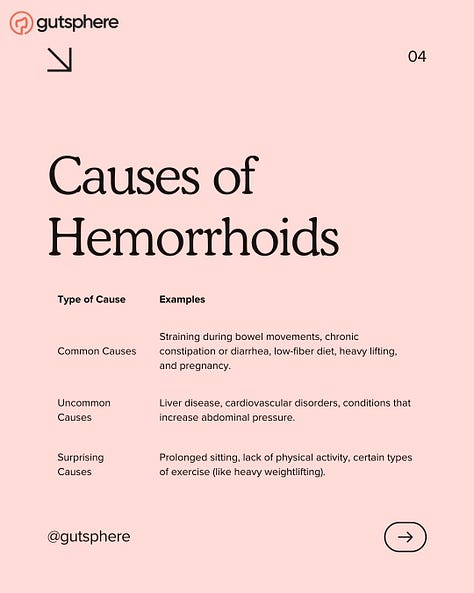
Straining during bowel movements: This is one of the most common causes of hemorrhoids. Straining increases pressure in the veins of the rectum and anus, causing them to swell.
Constipation: Chronic constipation can lead to straining, increasing the risk of developing hemorrhoids.
Pregnancy: The increased pressure on the pelvic veins during pregnancy can cause hemorrhoids. Additionally, the strain of childbirth can also contribute to their development.
Obesity: Excess body weight places additional pressure on the veins in the rectum and anus, increasing the risk of hemorrhoids.
Prolonged sitting: Sitting for extended periods, especially on the toilet, can increase pressure on the veins in the rectum and anus, contributing to hemorrhoid development.
Uncommon causes:
Liver disease: Cirrhosis or other liver diseases can lead to increased pressure in the veins of the rectum and anus, potentially causing hemorrhoids.
Tumors: Rectal or anal tumors can obstruct blood flow, leading to increased pressure and the development of hemorrhoids.
Controllable and Uncontrollable Risk Factors
Understanding the controllable and uncontrollable risk factors for hemorrhoids can help us take proactive steps to prevent or manage this condition.
Controllable risk factors:
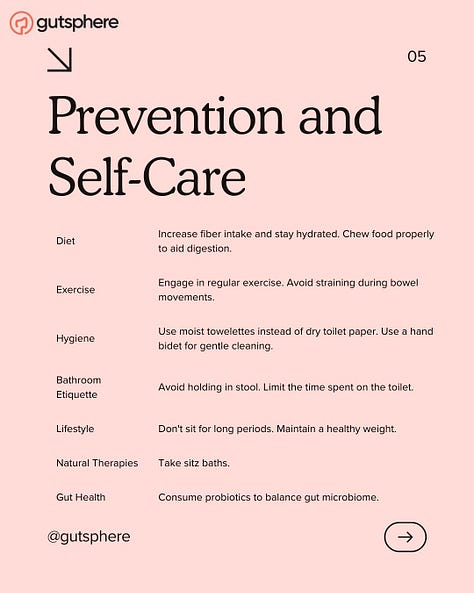
Diet: A low-fiber diet can contribute to constipation, which in turn can lead to straining and hemorrhoid development. By incorporating more fiber-rich foods into our diets, we can promote regular bowel movements and reduce the risk of hemorrhoids.
Hydration: Staying well-hydrated can help prevent constipation and reduce the risk of hemorrhoids. Aim for at least eight glasses of water per day, or more if you're physically active.
Exercise: Regular physical activity can help prevent constipation and promote healthy bowel movements. Aim for at least 30 minutes of moderate exercise, such as brisk walking, most days of the week.
Toilet habits: Avoid spending excessive time on the toilet or straining during bowel movements. Use a footstool to elevate your feet and promote a more natural squatting position while using the toilet.
Uncontrollable risk factors:
Age: The risk of developing hemorrhoids increases with age as the supporting tissues in the rectum and anus weaken over time.
Genetics: A family history of hemorrhoids can increase your risk of developing them. If your parents or grandparents have had hemorrhoids, you may be more likely to experience them as well.
Pregnancy: As mentioned earlier, pregnancy can increase the risk of hemorrhoids due to increased pressure on the pelvic veins. While pregnancy itself is not controllable, maintaining a healthy lifestyle and discussing any concerns with a healthcare professional can help manage the risk.
While age, genetics, and pregnancy are uncontrollable factors that can contribute to hemorrhoids, there are still several ways to minimize the risk and manage the condition. By adopting a proactive approach and focusing on modifiable factors, we can lessen the impact of uncontrollable elements on hemorrhoid development.
We have talked about hydration, nutrition, lifestyles interventions etc in our past editions of the newsletter that will improve gut health and subsequently should prevent hemorrhoids. We will revisit each of those in this edition in the context of hemorrhoids so that together, we can take charge of our health and tackle hemorrhoids head-on.
In conclusion, understanding the common and uncommon causes of hemorrhoids, as well as controllable and uncontrollable risk factors, can empower us to take preventive measures and manage this often-uncomfortable condition. By debunking myths and misconceptions, we can approach hemorrhoids with a clearer understanding and work towards better overall health.
Gut Microbiome and Hemorrhoids: "The Gut Connection: Microbiome's Role in Hemorrhoid Management"
When we think about hemorrhoids, the gut microbiome might not be the first thing that comes to mind. However, recent research has uncovered fascinating connections between the health of our gut and the development and management of hemorrhoids. In this section, we will delve into the relationship between gut health and hemorrhoids, exploring the latest scientific findings on the gut microbiome and its impact on this common but often misunderstood condition.
The Gut Microbiome: A Brief Overview
Our gut is home to trillions of microorganisms, including bacteria, viruses, fungi, and other microscopic life forms. Collectively, they make up our gut microbiome, which plays a vital role in digestion, nutrient absorption, immune function, and overall well-being. A balanced and diverse gut microbiome is essential for maintaining good health, while an imbalance or lack of diversity can lead to various health issues.
The Gut Microbiome and Hemorrhoids: The Connection
The gut microbiome can influence the development and management of hemorrhoids in several ways:
Bowel Regularity: A healthy gut microbiome promotes regular bowel movements, reducing the risk of constipation and straining, which can contribute to hemorrhoid development. Some strains of bacteria, such as Bifidobacterium and Lactobacillus, are particularly helpful in maintaining bowel regularity. We will talk about constipation in detail in later editions.
Inflammation: An imbalanced gut microbiome can lead to increased inflammation in the body, which can worsen hemorrhoid symptoms. On the other hand, a diverse and balanced microbiome helps regulate inflammation and supports overall gut health.
Immune Function: A well-functioning gut microbiome supports a robust immune system, which can help protect against infections that could potentially exacerbate hemorrhoids. For example, certain bacteria in the gut can help the immune system maintain a healthy balance between pro-inflammatory and anti-inflammatory responses.
Nutrient Absorption: Our gut microbiome plays a crucial role in the absorption of nutrients from the food we eat. Poor nutrient absorption, particularly of fiber, can contribute to constipation and hemorrhoids. A healthy gut microbiome can help ensure we absorb enough fiber and other essential nutrients for optimal digestion and bowel health.
Latest Research on Gut Microbiome and Hemorrhoids
Recent studies have highlighted the potential benefits of targeting the gut microbiome to prevent and manage hemorrhoids. Some key findings include:
Probiotics for hemorrhoid management: Probiotics are live microorganisms that can help restore a healthy balance to the gut microbiome when consumed in sufficient quantities. In a study conducted in 2019, participants with hemorrhoids who received a probiotic supplement experienced a significant reduction in pain, bleeding, and itching compared to those who received a placebo. This suggests that probiotics could potentially play a role in hemorrhoid management by promoting gut health.
Dietary fiber and gut health: A high-fiber diet has long been recommended for preventing and managing hemorrhoids. Fiber helps maintain regular bowel movements and soften stools, reducing strain on the rectal veins. Recent research has also shown that fiber plays a vital role in promoting gut health, as it serves as a food source for beneficial bacteria in the gut. This highlights the importance of a fiber-rich diet in both hemorrhoid prevention and gut health maintenance.
Fecal microbiota transplantation (FMT): While still an experimental treatment for various conditions, fecal microbiota transplantation (FMT) involves transferring the gut microbiome from a healthy donor to a recipient with an imbalanced gut microbiome. Some preliminary research has shown promising results in treating conditions such as inflammatory bowel disease and recurrent Clostridium difficile infections. Although more research is needed, FMT could potentially be explored as a treatment option for hemorrhoids in the future, as it aims to restore a healthy balance of gut microorganisms and improve overall gut health. We will talk about FMT in detail in the future editions.
Optimizing Gut Health to Manage Hemorrhoids
In our previous edition, we introduced the body as a machine framework, in which we elaborated how input, processing, and output impacts our gut health. Since then, we have talked comprehensively about Fiber, Fermented Food, Fodmap, Fasting, Fat, Exercises, Meditation, Breathing exercises, Water, Water Therapies, and many more.
We have linked to those editions. When you get time, please go through them.
As we conclude Part 1 of our comprehensive newsletter, we've gained valuable insights into the history, stages, causes, and the gut microbiome's role in hemorrhoids. This foundation of knowledge will serve as a springboard for our journey to effectively manage and prevent hemorrhoids in our daily lives.
Next
But the journey doesn't end here! In Part 2, we'll dive into the exciting world of lifestyle and self-care strategies. We'll explore a holistic approach to hemorrhoid prevention and management, focusing on the importance of nutrition, exercise, stress management, and bathroom etiquette. We'll equip you with practical tips and techniques to not only alleviate your symptoms but also improve your overall gut health.
So, stay tuned as we venture deeper into the world of hemorrhoids, empowering ourselves to take control of our health and well-being. Get ready for Part 2, where we'll reveal the secrets to conquering hemorrhoids and embracing a healthier lifestyle!
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
If you haven’t already subscribed then our sincere request, please subscribe.
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
gutsphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.