The Lifelong Impact: Antibiotics at Different Life Stages( Part 3/6)
Antibiotic Use at Different Life Stages: Impact on Gut Microbiome and Health
Welcome Back Gutsphere Friends,
Welcome, friends, to Part 3 of our series: "The Lifelong Impact: Antibiotics at Different Life Stages." This chapter takes us on a journey from conception to our golden years, delving into the intricate ways antibiotics impact us throughout our lives.
Ever wondered how antibiotics might shape our health over time? It's not just about that one-time effect. Antibiotics echo in our bodies for years, subtly influencing our health in ways we're just beginning to comprehend[1].
Interestingly, by the tender age of 3, our gut microbiome stabilizes to resemble an adult's[2]. Yet, the ripples of the antibiotics we've encountered throughout our lives continue to affect our health subtly but significantly.
In this part, we're not only investigating how antibiotics interact with our gut microbiome at different life stages, but we're also examining the potential links between antibiotics and diseases. Disturbances in the early-life gut microbiome may result in obesity, diabetes, and even neurological disorders[3]. We'll delve deeper into these aspects, but remember, correlation doesn't always mean causation!
Our goal is to navigate this complex field together, armed with the latest research and a thirst for understanding. So buckle up, friends, because the journey ahead promises to be as captivating as it is enlightening!
References
Temporal development of the gut microbiome in early childhood from the TEDDY study. (2018).https://www.nature.com/articles/s41586-018-0617-x
Selective maternal seeding and environment shape the human gut microbiome. https://pubmed.ncbi.nlm.nih.gov/29496731/
Microbiota in health and diseases, https://www.nature.com/articles/s41392-022-00974-4
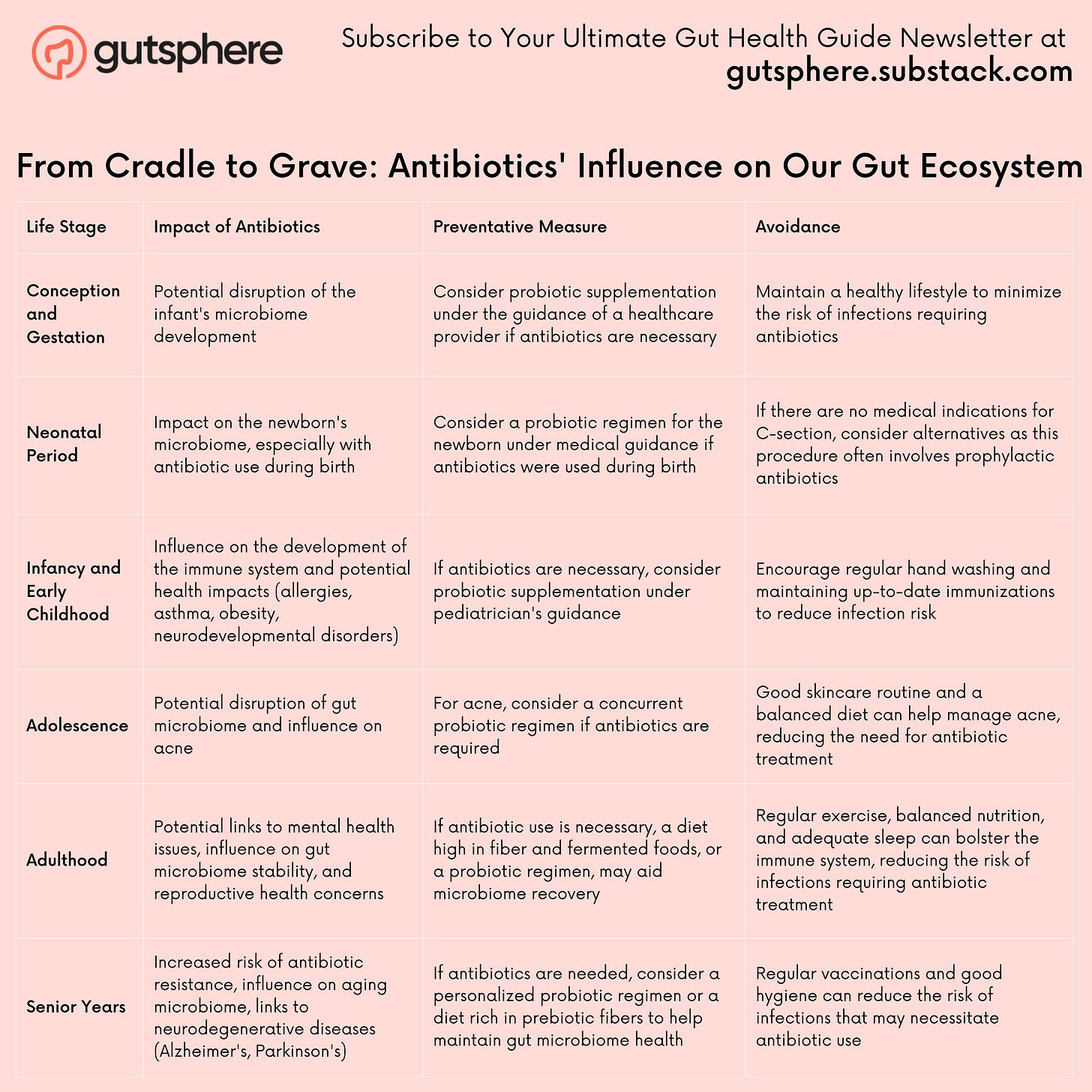
From Cradle to Grave: Antibiotics' Influence on Our Gut Ecosystem
Antibiotic Use at Different Life Stages: Impact on Gut Microbiome and Health
Let's navigate through the various stages of life, spotlighting the influence of antibiotics on our gut microbiome and health at each juncture.
Conception and Gestation: The First Encounter
Even before birth, we encounter antibiotics. If a mother takes antibiotics during pregnancy, these can cross the placenta, potentially impacting the developing baby's gut microbiome[1]. This early microbial disruption may have downstream effects on the child's immune development and susceptibility to diseases later in life[2].
The Neonatal Period: A Delicate Balance
In the early days of life, a baby's gut microbiome is a rapidly evolving landscape. Infants born through cesarean section or exposed to antibiotics around birth have been shown to have altered gut microbiomes compared to those born vaginally without antibiotic exposure[3]. These early changes could potentially influence the baby's health, affecting risks for allergies, asthma, or obesity[4].
Infancy and Early Childhood: Setting the Stage
As children grow and their immune system develops, antibiotics can dramatically reshape their gut microbiome. A landmark study by Korpela and colleagues (2020)[5]] showed that antibiotic use in the first years of life could lead to long-lasting changes in the gut microbiome. Disruptions in this critical period could potentially influence susceptibility to autoimmune conditions, mental health, and metabolic disorders[5].
Adolescence: A Time of Change
The teenage years are a period of dynamic physiological changes, and the gut microbiome is no exception. Antibiotics, commonly prescribed for conditions like acne, can disrupt this delicate balance. Research indicates that alterations in the adolescent microbiome might impact not just gut health but also mental wellbeing[6].
Adulthood: Consequences and Connections
In adulthood, the microbiome typically achieves a degree of stability. However, antibiotic use can still cause significant disturbances. Studies have linked changes in the adult microbiome due to antibiotics with an increased risk of mental health disorders and metabolic conditions like obesity and diabetes[7].
Senior Years: A Balancing Act
In our golden years, our microbiome changes again, often becoming less diverse. Antibiotics can exacerbate this, increasing the risk of antibiotic-resistant infections, which are a significant concern in this age group[8]. Moreover, some evidence suggests that microbiome changes might be linked with neurodegenerative conditions like Alzheimer's and Parkinson's diseases[9].
Remember, while we've highlighted potential risks associated with antibiotic use, these drugs are vital tools in fighting bacterial infections. The aim is not to incite fear but to encourage informed discussions about antibiotic use at different life stages. Always consult healthcare professionals for personalized advice.
References
Stokholm J, Blaser MJ, Thorsen J, et al. Maturation of the gut microbiome and risk of asthma in childhood. https://www.nature.com/articles/s41467-017-02573-2
Mueller NT, Bakacs E, Combellick J, Grigoryan Z, Dominguez-Bello MG. The infant microbiome development: mom matters. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4464665/
Dominguez-Bello MG, Costello EK, Contreras M, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. https://pubmed.ncbi.nlm.nih.gov/20566857/
Tun MH, Konya T, Takaro TK, et al. Exposure to household furry pets influences the gut microbiota of infants at 3-4 months following various birth scenarios. Microbiome. https://pubmed.ncbi.nlm.nih.gov/28381231/
Korpela K, Costea P, Coelho LP, et al. Selective maternal seeding and environment shape the human gut microbiome. https://pubmed.ncbi.nlm.nih.gov/29496731/
Mangiola F, Ianiro G, Franceschi F, Fagiuoli S, Gasbarrini G, Gasbarrini A. Gut microbiota in autism and mood disorders. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698498/
Cho I, Yamanishi S, Cox L, et al. Antibiotics in early life alter the murine colonic microbiome and adiposity. https://www.nature.com/articles/nature11400
Claesson MJ, Jeffery IB, Conde S, et al. Gut microbiota composition correlates with diet and health in the elderly. https://www.nature.com/articles/nature11319
Minter MR, Zhang C, Leone V, et al. Antibiotic-induced perturbations in gut microbial diversity influences neuro-inflammation and amyloidosis in a murine model of Alzheimer’s disease. https://www.nature.com/articles/srep30028
Through the Ages: Minimizing Antibiotics' Impact on Your Microbiome
Navigating the intricate web of our microbiome is a complex journey, made even more challenging by the delicate balance we need to strike with antibiotics. From conception to our golden years, the choices we make can significantly influence this balance and, in turn, our health. Here's a comprehensive guide to understanding how we can mitigate the impact of antibiotics on our microbiome at different stages of life.
Conception and Gestation
Preventative Measure: Avoid unnecessary antibiotic use during pregnancy. If antibiotics are necessary, consider supplementing with probiotics after consultation with a healthcare provider.
Avoidance: Maintain a healthy lifestyle to minimize the risk of infections that might require antibiotics.
Neonatal Period
Preventative Measure: If antibiotics are used during birth, a probiotic regimen might help restore the newborn's microbiome. This should always be discussed with a healthcare provider.
Avoidance: Consider alternatives to C-sections if there are no medical indications for it, as this procedure often involves prophylactic antibiotics.
Infancy and Early Childhood
Preventative Measure: If antibiotics are necessary in early childhood, consider probiotic supplementation under the guidance of a pediatrician.
Avoidance: Regular hand washing and maintaining up-to-date immunizations can help reduce infection risk and, by extension, antibiotic use.
Adolescence
Preventative Measure: For acne, explore topical treatments or other non-antibiotic options first. If antibiotics are required, consider a concurrent probiotic regimen, with medical guidance.
Avoidance: Good skincare routine and a balanced diet can help manage acne, reducing the need for antibiotic treatment.
Adulthood
Preventative Measure: If antibiotic use is necessary, a diet high in fiber and fermented foods, or a probiotic regimen, may aid microbiome recovery.
Avoidance: Regular exercise, balanced nutrition, and adequate sleep can bolster the immune system, reducing the risk of infections requiring antibiotic treatment.
Senior Years
Preventative Measure: Careful use of antibiotics, under strict medical guidance, is important. If antibiotics are needed, consider a personalized probiotic regimen or a diet rich in prebiotic fibers to help maintain gut microbiome health.
Avoidance: Regular vaccinations and good hygiene can reduce the risk of infections that may necessitate antibiotic use.
Overall Strategy: The Holistic Approach
Throughout all stages of life, a holistic approach to health is beneficial. This includes stress management, regular physical activity, balanced nutrition, and exposure to diverse microbes in nature for a healthier microbiome .
Moreover, individual differences should be considered. Everyone's microbiome is unique, thus, responses to antibiotics and strategies to mitigate their effects will vary. Also, prebiotics, the 'food' for our gut microbes, are as crucial as probiotics in maintaining and restoring a healthy gut microbiome.
Emerging strategies like Fecal Microbiota Transplant (FMT) show promise in treating conditions related to gut microbiome disruptions from antibiotic use. But it's still an area of ongoing research.
Remember, while these measures can mitigate the impacts of antibiotics, they can't entirely eliminate them. Always seek advice from healthcare professionals for personalized guidance.
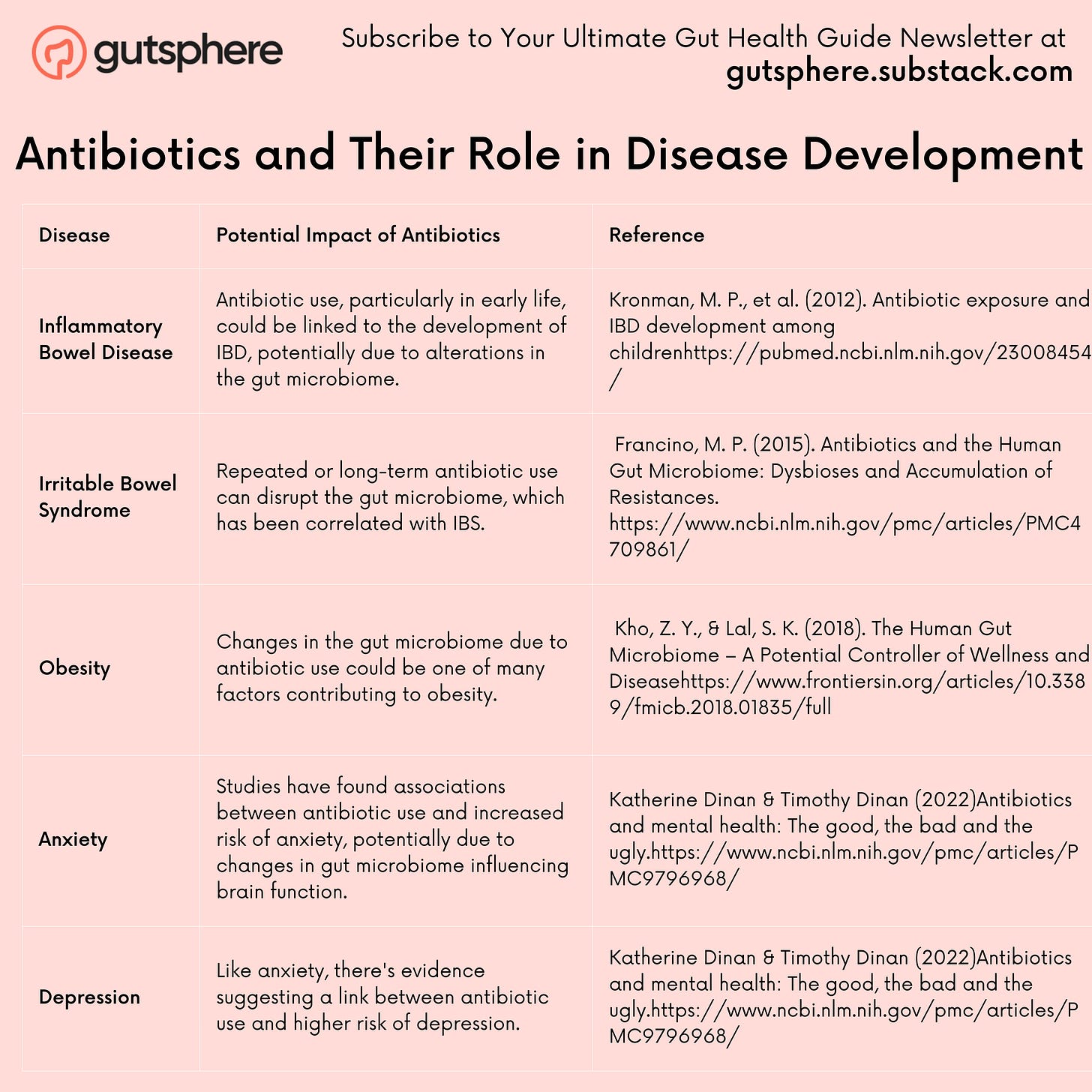
Antibiotics and Disease Links
Let's embark on this fascinating deep dive into the links between antibiotics and disease. As we navigate through this labyrinth of interconnected topics, we'll shed light on both digestive and mental health impacts, a realm that is only now beginning to come into public awareness.
Cracking the Code: Antibiotics and Their Role in Disease Development
Antibiotics and Digestive Diseases
Our first stop is our gut, home to trillions of microbes that constitute our microbiome. It is becoming increasingly clear that the health of our microbiome is intimately linked with our overall health. Researchers have found correlations between alterations in the gut microbiome and digestive diseases such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and even obesity[1].
The role of antibiotics in this story? Antibiotics, particularly when used repeatedly or over long periods, can significantly disrupt the delicate balance of our gut microbiome, potentially paving the way for digestive diseases[2]. For example, several studies have indicated a possible link between antibiotic use in early life and later development of IBD[3]].
However, it's important to note that correlation does not equal causation. While these studies suggest a link, they don't definitively prove that antibiotics cause these diseases. Other factors, including genetics and diet, also play significant roles. Thus, a comprehensive understanding requires more research in this field.
Antibiotics and Mental Health
Now, let's navigate to a surprising arena where antibiotics might hold sway – our brains. The concept of a gut-brain axis, a two-way communication highway linking our digestive system with our brain, is gaining traction in scientific circles[4].
Evidence suggests that alterations in the gut microbiome, like those resulting from antibiotic use, might influence mental health. For instance, several studies have shown an association between antibiotic use and increased risk of anxiety and depression[5]. This might be because our gut microbes produce a variety of substances, including neurotransmitters and short-chain fatty acids, which can impact brain function[6].
Again, we need to tread carefully here. While these findings are intriguing, they're far from conclusive. The microbiome-brain interaction is complex and not yet fully understood. So, while antibiotics may have a role, they are just one part of a larger, intricate puzzle.
The key takeaway from this journey? Antibiotics are powerful tools in our medical arsenal, but their use is not without consequences. As we unravel the complexities of our microbiome and its interactions with our health, we underscore the need for a balanced, judicious approach to antibiotic use. The journey of understanding is far from over, but we're making promising strides in the right direction.
References
The human gut microbiome – a potential controller of wellness and disease. https://doi.org/10.3389/fmicb.2018.01835
Antibiotics and the Human Gut Microbiome: Dysbioses and Accumulation of Resistances. https://doi.org/10.3389/fmicb.2015.01543
Antibiotic exposure and IBD development among children: a population-based cohort study. https://doi.org/10.1542/peds.2011-3886
Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. https://doi.org/10.1038/nrn3346
Antibiotic exposure and the risk for depression, anxiety, or psychosis: a nested case-control study. https://doi.org/10.4088/JCP.15m09961
Neurotransmitter modulation by the gut microbiota. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6005194/
Conclusion for Part 3
As we wrap up Part 3, it's apparent how deeply antibiotics have infiltrated our lives, from conception to our twilight years. They've become a cornerstone of modern medicine, yet their unseen impact on our gut microbiome and, by extension, our overall health can be profound. The links between antibiotics and various diseases, both mental and digestive, underscore the need for careful consideration before we introduce these potent drugs into our bodies.
However, it's also clear that not all hope is lost. By implementing preventative measures and health-conscious habits, we can potentially mitigate some of these effects. It's all about finding balance—understanding when antibiotics are truly necessary and taking steps to protect and restore our microbiome when they are.
Next Part 4 Informed Decisions: Antibiotics - Yes or No?
But now, a pressing question looms: How can we make informed decisions about antibiotic use? Should we be saying "yes" or "no" to these medications? And how do we navigate these complex discussions with our healthcare providers?
Hold on to these questions, friends, because in Part 4, we'll arm ourselves with the knowledge we need to navigate these crucial decisions. We'll be delving into the things you need to know before taking antibiotics and discussing the trade-offs that need to be considered. It's time for us to seize control of our health and make empowered, informed decisions. So, stay tuned for the next enlightening journey in Part 4—"Informed Decisions: Antibiotics - Yes or No?" Your compass for this complex terrain is on its way!
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
If you haven’t already subscribed then our sincere request, please subscribe.
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
GutSphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.