The Science of Allergies: Hygiene Hypothesis and the Gut Microbiome( Part 2/5)
Deconstructing the Hygiene Hypothesis: An Examination of Cleanliness, Imbalance, and Allergy Emergence
Breaking Down the Hygiene Hypothesis: Its Implications for Allergies
The Research Landscape: The Gut Microbiome and Allergies
The Dark Side of Imbalance: Dysbiosis and its Role in Allergies
Introduction:
Welcome back to our enlightening journey as we continue to dissect the fascinating world of allergies and the gut microbiome. In the first part of this series, we embarked on a quest to unravel the complex connection between the surge in allergy prevalence and the intricate ecosystem of microorganisms in our gut. We laid the groundwork of understanding allergies and their myriad forms and grappled with the mysteries of our gut microbiome and its profound influence on our health.
As we step into Part 2 of our series, titled "The Science of Allergies: Hygiene Hypothesis and the Gut Microbiome," we stand on the precipice of an intriguing paradox. We find ourselves asking, could our pursuit of cleanliness be contributing to the rise in allergies?
The answer may lie in a controversial yet thought-provoking concept known as the 'Hygiene Hypothesis.' This hypothesis suggests that our modern lifestyle, with its emphasis on cleanliness and sanitation, may inadvertently be disrupting the balance of our gut microbiome, impacting our immune system and possibly heightening our susceptibility to allergies. A seemingly counterintuitive idea, isn't it? The theory that perhaps we might be 'too clean for our own good' takes us down a path that encourages us to reexamine our relationship with the microbial world around and within us.
This part of our journey will dive into the depths of this hypothesis, breaking it down piece by piece to reveal its implications on our understanding of allergies. We will investigate the research landscape, looking at the latest findings that connect the gut microbiome to allergies, and discover the dark side of imbalance - dysbiosis - and its role in allergic conditions.
The journey ahead is filled with challenges and revelations as we tackle some of the most thought-provoking questions in the realm of allergy science. As we navigate this complex territory together, we look forward to uncovering the dynamic interplay between our environment, our lifestyle, and our gut microbiome, reshaping our understanding of health and wellbeing.
Are we ready to question our assumptions, to challenge our preconceptions, and to delve deeper into the world of allergies and the gut microbiome? Let's embark on this journey of discovery together in Part 2: The Science of Allergies!
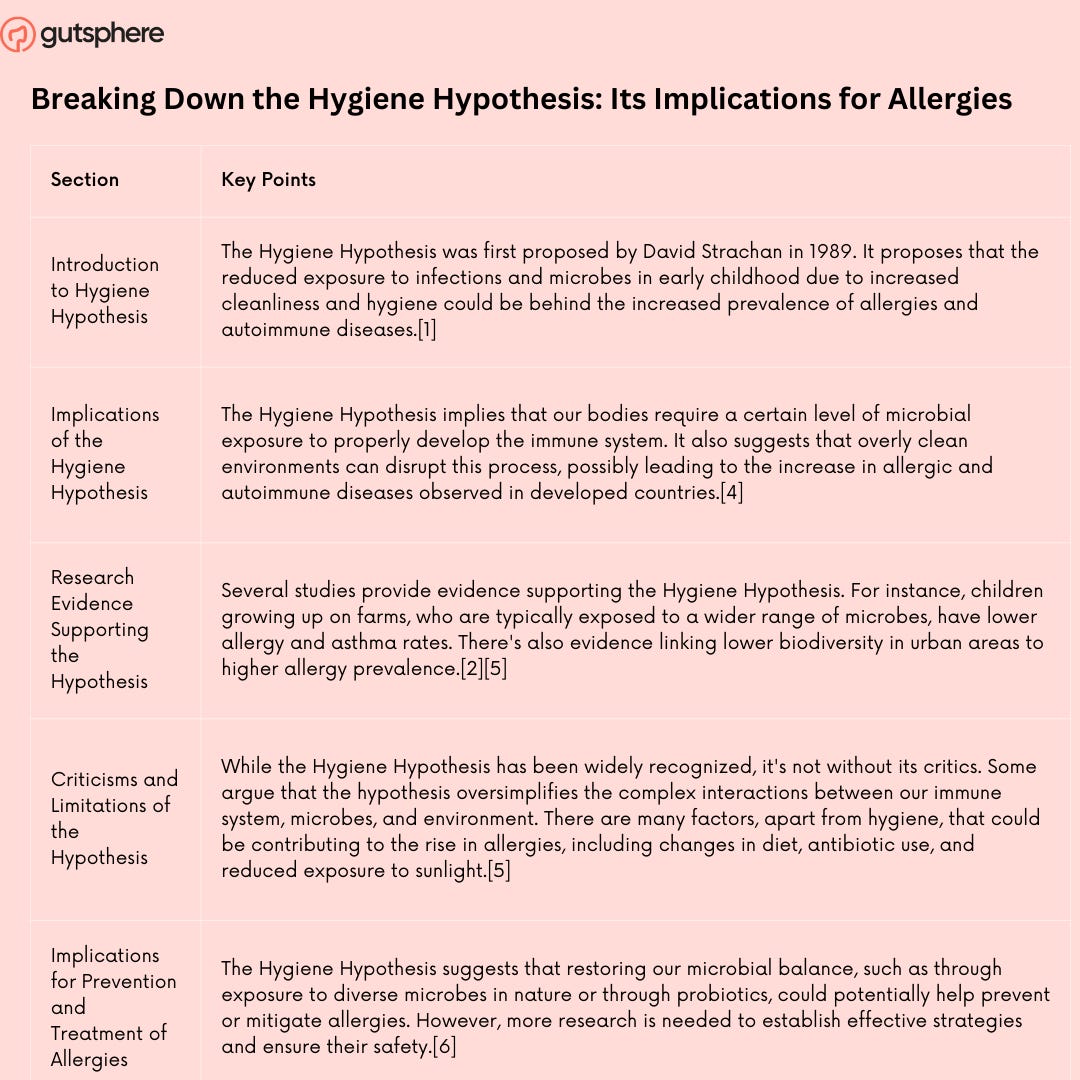
Breaking Down the Hygiene Hypothesis: Its Implications for Allergies
The Hygiene Hypothesis: a concept that first graced scientific literature in the late 20th century, which has since fueled a wave of fascinating and often contentious discourse within the scientific community. First proposed by epidemiologist David P. Strachan in a seminal 1989 paper, the Hygiene Hypothesis posits that the decreasing incidence of infections in western countries and the simultaneous increase in allergic diseases is a result of a reduced exposure to infectious agents during early childhood[1].
So, what exactly does the Hygiene Hypothesis mean for us, especially in the context of allergies? Let's embark on this journey to deconstruct this theory and analyze its implications.
Strachan's initial observation stemmed from an interesting correlation: children from larger families had lower rates of hay fever and eczema. This counter-intuitive finding led to the proposition that increased exposure to infectious agents via unhygienic contact with older siblings protected these children from developing allergic diseases[1].
The Hygiene Hypothesis revolves around our immune system, an intricate network of cells, tissues, and organs that acts as a stalwart defender against foreign invaders. This defense mechanism is bifurcated into two primary responses: Th1 and Th2. Th1 responses are typically geared towards fighting viruses and bacteria, whereas Th2 responses combat parasites. In the context of allergies, it's the overactive Th2 responses to typically harmless substances, like pollen or certain foods, that lead to allergic reactions[2].
The Hygiene Hypothesis suggests that our immune system's equilibrium is dependent on regular interactions with diverse microorganisms and parasites, primarily during our formative years. By exposing ourselves to a broad spectrum of microbes, we 'train' our immune system to distinguish between harmful pathogens and harmless allergens, thus mitigating overactive Th2 responses[3].
Modern living standards, marked by advanced sanitation, widespread use of antibiotics, smaller family sizes, and changes in dietary habits, have arguably led to decreased microbial exposure. This sanitization of our environment, according to the Hygiene Hypothesis, might be disrupting the necessary immune training, skewing our immune responses towards the Th2 type, and hence, increasing our susceptibility to allergies[4].
The Hygiene Hypothesis received further support from studies highlighting the lower prevalence of allergies in individuals raised in farm environments. The 'farm effect,' as it's commonly referred to, points to the protective effects of rich microbial exposure through regular contact with farm animals, consumption of unpasteurized milk, and minimal antibiotic use[5].
As intriguing as the Hygiene Hypothesis is, it's important for us to approach it with a balanced perspective. While it's provided a framework to understand the escalating prevalence of allergies in western countries, it's not without limitations. For one, it doesn't fully explain why some people develop allergies later in life or why certain individuals are more susceptible to allergies despite growing up in microbe-rich environments[6].
Additionally, the initial Hygiene Hypothesis primarily concerned infectious agents and didn't account for the role of our gut microbiota, a critical component of our immune system's education. Recognizing this, the hypothesis has been refined over the years into the 'Microbial Diversity Hypothesis,' which posits that a diverse microbial exposure, particularly during infancy and early childhood, is key to a well-regulated immune system[7].
In conclusion, the Hygiene Hypothesis, while not a comprehensive explanation for the rise in allergies, offers valuable insights into the complex interplay between our immune system, our environment, and our lifestyle. By encouraging us to reevaluate our relationship with the microbial world, it's propelling research into exciting new directions, such as probiotics and helminthic therapy, aimed at restoring our microbial balance and potentially mitigating allergy prevalence. The hypothesis certainly challenges our conventional wisdom and urges us to find a healthier balance between hygiene and our body's need for microbial interaction.
References
Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989 Nov 18;299(6710):1259-60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1838109/ .
Romagnani S. The increased prevalence of allergy and the hygiene hypothesis: missing immune deviation, reduced immune suppression, or both? Immunology. 2004 May;112(3):352-63.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1782506/
Bach JF. Revisiting the Hygiene Hypothesis in the Context of Autoimmunity .https://www.frontiersin.org/articles/10.3389/fimmu.2020.615192/full .
Bloomfield SF, Stanwell-Smith R, Crevel RW, Pickup J. Too clean, or not too clean: the Hygiene Hypothesis and home hygiene. Clin Exp Allergy. 2006 Apr;36(4):402-25. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1448690/
Ege MJ, Mayer M, Normand AC, Genuneit J, Cookson WO, Braun-Fahrländer C, Heederik D, Piarroux R, von Mutius E; GABRIELA Transregio 22 Study Group. Exposure to environmental microorganisms and childhood asthma. N Engl J Med. 2011 Feb 24;364(8):701-9.https://pubmed.ncbi.nlm.nih.gov/21345099/
von Hertzen LC, Haahtela T. Disconnection of man and the soil: reason for the asthma and atopy epidemic? J Allergy Clin Immunol. 2006 Feb;117(2):334-44. https://pubmed.ncbi.nlm.nih.gov/16461134/
Hanski I, von Hertzen L, Fyhrquist N, Koskinen K, Torppa K, Laatikainen T, Karisola P, Auvinen P, Paulin L, Mäkelä MJ, Vartiainen E, Kosunen TU, Alenius H, Haahtela T. Environmental biodiversity, human microbiota, and allergy are interrelated. Proc Natl Acad Sci U S A. 2012 May 22;109(21):8334-9. doi: 10.1073/pnas.1205624109. Epub 2012 May 7. https://www.pnas.org/doi/10.1073/pnas.1205624109
The Research Landscape: The Gut Microbiome and Allergies
The intricacies of human health are dictated by an unexpected source—the tiny microbial inhabitants of our gut, collectively known as the gut microbiome. These microscopic lifeforms have begun to take center stage in recent years, revealing their profound influence on an array of health conditions, including allergies. In this chapter, we shall delve deeper into the research landscape concerning the gut microbiome and allergies, underscoring the pivotal role these unseen organisms play in our immune responses.
The gut microbiome consists of trillions of microbes, primarily bacteria, but also includes viruses, fungi, and protozoa, each contributing to the health and functioning of the human body in their unique ways[1]. With around 70% of the body's immune cells residing in the gut, there is a profound interaction between the microbiome and the immune system[2]. This interaction helps shape immune responses, including those to allergens, giving us a new lens through which to understand and potentially address allergic conditions.
One of the critical features of the gut microbiome, particularly relevant to allergies, is its diversity. A higher diversity of gut microbes is generally associated with better health outcomes[3]. Studies have found that individuals with certain allergic conditions, such as atopic dermatitis and food allergies, often have a less diverse gut microbiome compared to those without these conditions[4,5]. This lack of diversity may weaken the immune system's ability to distinguish between harmful and harmless substances, leading to overactive immune responses when exposed to allergens.
One groundbreaking study that helped establish the connection between the gut microbiome and allergies is the work by Stefka et al. in 2014[6]. In this study, mice that were sensitized to peanut allergens were fed a particular strain of bacteria, Clostridia. This bacterial treatment prevented the mice from having allergic reactions to peanuts. The researchers found that the bacteria prompted the production of a type of immune cell that promoted tolerance to food allergens. This pivotal study underscored the potential of modulating the gut microbiome to prevent and manage food allergies.
Further research is elucidating the role of early-life gut microbiome composition in allergy risk. The CHILD study, a large birth cohort study in Canada, found that infants at risk of asthma had different gut microbiota compared to those not at risk[7]. A similar pattern has been observed with food allergies. A study by Feehley et al. found that infants with food allergies had distinct gut microbiota compared to those without allergies[8].
Intriguingly, a mother's microbiome during pregnancy might also influence her child's allergy risk. Studies suggest that microbial exposure in utero could have lasting impacts on the infant's immune system[9]. However, more research is needed to understand these maternal-infant microbiome dynamics and their implications for allergies.
While these findings provide compelling evidence for the gut microbiome-allergy connection, it's important to remember that the microbiome is just one piece of the complex puzzle of allergies. Factors such as genetics, diet, environmental exposures, and lifestyle all interplay with the microbiome to shape our immune responses.
One promising avenue of research is leveraging our understanding of the gut microbiome to develop new treatments for allergies. This could include probiotics, prebiotics, or even fecal microbiota transplantation[10]. However, we still have much to learn about which specific microbial alterations are beneficial, how to best implement these changes, and what potential risks might be involved.
In conclusion, the emerging research landscape paints an intriguing picture of the gut microbiome's role in allergies. It suggests that by supporting a balanced, diverse gut microbiome, we might be able to improve our immune responses and reduce allergy risk. As we continue to unravel the mysteries of our gut microbiome, we may unlock new strategies to prevent and manage allergies, shaping a healthier future for us all.
Here's a summary of the chapter "The Research Landscape: The Gut Microbiome and Allergies" in a tabular format:
References
Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J. 2017 May 16;474(11):1823-1836. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5433529/
Vighi G, Marcucci F, Sensi L, Di Cara G, Frati F. Allergy and the gastrointestinal system. Clin Exp Immunol. 2008 Sep;153 Suppl 1(Suppl 1):3-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2515351/ .
Lynch SV, Pedersen O. The Human Intestinal Microbiome in Health and Disease. N Engl J Med. 2016 Dec 15;375(24):2369-2379. https://pubmed.ncbi.nlm.nih.gov/27974040/
Song H, Yoo Y, Hwang J, Na YC, Kim HS. Faecalibacterium prausnitzii subspecies-level dysbiosis in the human gut microbiome underlying atopic dermatitis. J Allergy Clin Immunol. 2016 Mar;137(3):852-860. https://pubmed.ncbi.nlm.nih.gov/26431583/ .
Bunyavanich S, Shen N, Grishin A, Wood R, Burks W, Dawson P, Jones SM, Leung DYM, Sampson H, Sicherer S, Clemente JC. Early-life gut microbiome composition and milk allergy resolution. J Allergy Clin Immunol. 2016 Oct;138(4):https://pubmed.ncbi.nlm.nih.gov/27292825/
Stefka AT, Feehley T, Tripathi P, Qiu J, McCoy K, Mazmanian SK, Tjota MY, Seo GY, Cao S, Theriault BR, Antonopoulos DA, Zhou L, Chang EB, Fu YX, Nagler CR. Commensal bacteria protect against food allergen sensitization. Proc Natl Acad Sci U S A. 2014 Sep 9;111(36):13145-50. https://pubmed.ncbi.nlm.nih.gov/25157157/ .
Arrieta MC, Stiemsma LT, Dimitriu PA, Thorson L, Russell S, Yurist-Doutsch S, Kuzeljevic B, Gold MJ, Britton HM, Lefebvre DL, Subbarao P, Mandhane P, Becker A, McNagny KM, Sears MR, Kollmann T; CHILD Study Investigators, Mohn WW, Turvey SE, Brett Finlay B. Early infancy microbial and metabolic alterations affect risk of childhood asthma. https://pubmed.ncbi.nlm.nih.gov/26424567/
Feehley T, Plunkett CH, Bao R, Choi Hong SM, Culleen E, Belda-Ferre P, Campbell E, Aitoro R, Nocerino R, Paparo L, Andrade J, Antonopoulos DA, Berni Canani R, Nagler CR. Healthy infants harbor intestinal bacteria that protect against food allergy. Nat Med. 2019 Mar;25(3):448-453. https://www.nature.com/articles/s41591-018-0324-z
Vuillermin PJ, Macia L, Nanan R, Tang ML, Collier F, Brix S. The maternal microbiome during pregnancy and allergic disease in the offspring. Semin Immunopathol. 2017 Sep;39(6):669-675. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5711986/
Zimmermann P, Curtis N. The influence of the intestinal microbiome on vaccine responses. Vaccine. 2018 Jul 16;36(30):4433-4439. https://pubmed.ncbi.nlm.nih.gov/29909134/
The Dark Side of Imbalance: Dysbiosis and its Role in Allergies
The gut microbiome, this mysterious ecosystem within us, has profound effects on our health, dictating the balance between health and disease. As we delve deeper into this invisible universe, we're beginning to uncover the dark side of this balance: the state of dysbiosis. Dysbiosis, a term denoting an imbalance or maladaptation in our microbiota, is increasingly being linked to a wide range of health issues, including allergies. In this chapter, we'll examine the unsettling impact of dysbiosis and its role in allergies, backed by scientific evidence.
Our gut microbiota are generally resilient. However, factors such as diet, lifestyle, medication usage, and stress can disturb this harmony, tipping the scales towards dysbiosis [1]. A lack of diversity or an overabundance of certain bacterial species, both hallmarks of dysbiosis, can impair the gut's protective barrier, disrupt immune regulation, and promote inflammation, setting the stage for allergic disorders [2].
Several studies have unveiled correlations between gut dysbiosis and the development of allergies. One investigation of infants showed that those who developed allergies by age two had different gut microbiota compositions early in life, signifying that dysbiosis could be a risk factor for allergies [3]. Moreover, research has demonstrated that children with food allergies have distinct gut microbiota compared to non-allergic children, further linking dysbiosis with allergy development [4].
Evidence also suggests that dysbiosis may play a role in respiratory allergies. For example, a study involving children with asthma found lower bacterial diversity in their gut microbiota, compared to healthy controls [5]. Similarly, gut dysbiosis has been identified in patients with allergic rhinitis, another prevalent respiratory allergy [6].
Another angle from which we can appreciate the link between dysbiosis and allergies is by observing the effect of probiotics, live bacteria and yeasts beneficial for our health. Certain probiotics can potentially restore a healthy microbiota balance and improve allergic symptoms. For instance, certain strains of Lactobacillus and Bifidobacterium have demonstrated promising results in managing eczema, a common allergic skin disorder [7]. Nevertheless, while the potential of probiotics is enticing, more extensive and detailed research is needed to confirm their efficacy and understand their mechanism of action fully.
In conclusion, an intricate network of interactions ties together dysbiosis and allergies, accentuating the importance of maintaining our microbial balance. The gut microbiome's critical role in immune regulation makes it a likely protagonist in the allergy saga, but there is still much we need to understand. Our quest to decipher the complexities of dysbiosis and its implications for allergies is only just beginning. As we continue to explore this fascinating frontier, we hope to unveil therapeutic strategies that will help us reclaim our internal equilibrium and ward off allergies.
References
[1] Carding, Simon, et al. "Dysbiosis of the gut microbiota in disease." Microbial Ecology in Health & Disease vol. 26 (2015). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4315779/
[2] Cenit, Maria Carmen, et al. "Intestinal Dysbiosis and Rheumatoid Arthritis: A Link between Gut Microbiota and the Pathogenesis of Rheumatoid Arthritis." Journal of Immunology Research vol. 2017 (2017). https://pubmed.ncbi.nlm.nih.gov/28948174/
[3] Arrieta, Marie-Claire, et al. "Early infancy microbial and metabolic alterations affect risk of childhood asthma." Science Translational Medicine vol. 7, no. 307 (2015). https://pubmed.ncbi.nlm.nih.gov/26424567/
[4] Fazlollahi, M., et al. "The nasal microbiome in asthma." Journal of Allergy and Clinical Immunology vol. 142, no. 3 (2018). https://pubmed.ncbi.nlm.nih.gov/29518419/
[5] Abrahamsson, Thomas R., et al. "Low diversity of the gut microbiota in infants with atopic eczema." Journal of Allergy and Clinical Immunology vol. 129, no. 2 (2012). https://pubmed.ncbi.nlm.nih.gov/22153774/
[6] Ipci, Kagan, et al. "The possible mechanisms of the human microbiome in allergic diseases." European Archives of Oto-Rhino-Laryngology vol. 274, no. 2 (2017). https://pubmed.ncbi.nlm.nih.gov/27115907/
[7] Zuccotti, Gian Vincenzo, et al. "Probiotics for prevention of atopic diseases in infants: systematic review and meta-analysis." Allergy vol. 70, no. 11 (2015). https://pubmed.ncbi.nlm.nih.gov/26198702/
Conclusion
In our exploration of the gut microbiome-allergy connection in Part 2, we've journeyed through some compelling domains of modern medical research. We've investigated the hygiene hypothesis, understanding its implications for the rise of allergies. It seems that our societal inclination towards excessive cleanliness might have inadvertently disrupted the ancient bond between us and our microbial allies, contributing to the surge in allergies.
We delved into the intriguing world of our gut microbiome, appreciating its profound influence on our health and wellbeing. The gut microbiome's role in our immune function and allergy development is fascinating. Imbalance or dysbiosis in our gut microbiome can potentially precipitate a cascade of immune dysregulation, leading to allergies and other immune-related conditions.
The complex relationship between our gut microbiome and allergies indeed paints a compelling narrative. However, it's important to remember that this is a dynamic and rapidly evolving field of research. There's still much to learn, much to explore, and much to understand.
Next Part 3: The Traditional Wisdom: Insights from the Past and Present Strategies for Allergy Management
As we pull the curtain on Part 2, it's clear that we are just beginning to understand the gut microbiome's role in allergies. This knowledge inspires us to look towards both the past and the future for solutions. In Part 3, we will navigate through the intriguing avenues of traditional wisdom, modern strategies, and promising interventions to manage allergies and restore our gut health.
We will unearth ancient insights and modern practices that could potentially nurture our gut microbiome and tame allergies. We will explore the conventional medical approaches and lifestyle interventions, understanding their roles in managing allergies and promoting a balanced, diverse microbiome. And we will delve into the promising world of probiotics and prebiotics, appreciating their potential in restoring a healthy microbiome and reducing allergies.
So, stay with us as we embark on this exciting journey in Part 3: "The Traditional Wisdom: Insights from the Past and Present Strategies for Allergy Management." From age-old practices to cutting-edge research, we will explore how we can cultivate a healthier relationship with our invisible allies and harness their potential for our health and wellbeing. The best is yet to come!
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
If you haven’t already subscribed then our sincere request, please subscribe.
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Thank You
gutsphere Team
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.