Understanding Your Colonoscopy Results ( Part 7/10)
Guidance on interpreting colonoscopy results, common findings, and the significance of follow-up screenings
Introduction: Unveiling the Mysteries Behind Your Colonoscopy
Greetings, Gutsphere community! In the much-anticipated sixth edition of our series, we delve into an essential phase of your colonoscopy journey—interpreting the results. Understanding what your findings mean is crucial in navigating the next steps in your colorectal health management. With clarity and insight, we aim to demystify your colonoscopy results, guiding you through common findings, potential follow-up procedures, and reinforcing the importance of regular screenings in maintaining optimal colon health.
Navigating Your Colonoscopy Results
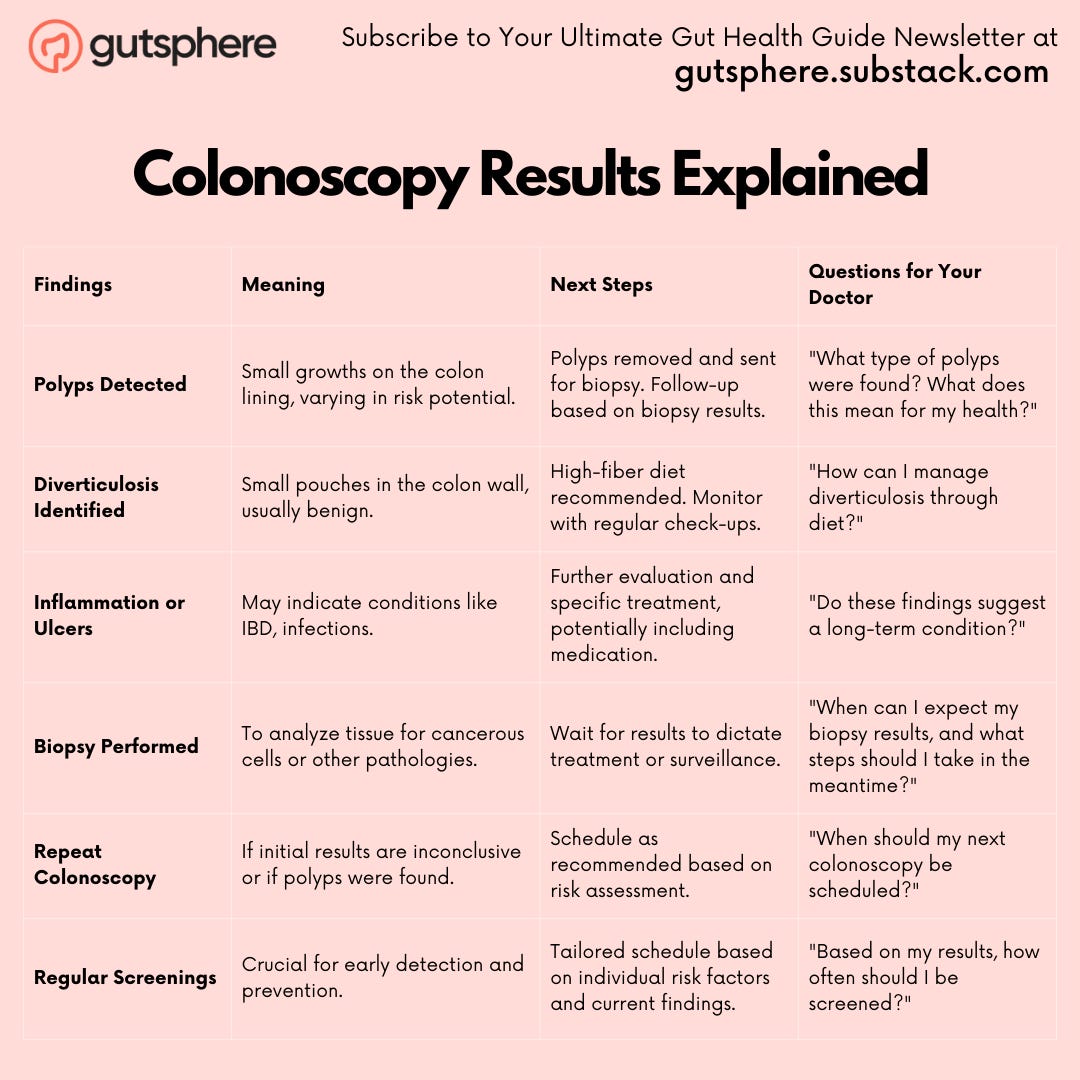
A colonoscopy is a critical diagnostic tool in gastrointestinal health, providing insights that can guide preventive strategies and treatment plans for various conditions. Upon receiving colonoscopy results, patients often encounter terms like polyps, diverticulosis, and inflammation or ulcers. Understanding these common findings and their implications is essential for navigating the next steps in managing your health.
1. Common Findings and Their Implications
Polyps: The Prevalent Findings
Overview and Types
Polyps, small growths on the colon lining, are among the most common findings during a colonoscopy. They vary widely in size, shape, and histology, with types including adenomatous (precancerous), hyperplastic (generally noncancerous), and sessile serrated polyps.
Implications
While most polyps are benign, their presence can increase the risk of developing colorectal cancer, especially if they are adenomatous. The size and number of polyps can also influence this risk; larger polyps and those in greater numbers are more concerning.
Next Steps
Polyps are usually removed during the colonoscopy procedure through a process called polypectomy. Following removal, polyps are sent for histological examination to determine their type and potential for malignancy. This analysis dictates follow-up care, ranging from routine surveillance to more immediate interventions if high-risk features are identified.
Diverticulosis: A Common Condition
Overview
Diverticulosis is characterized by the formation of small pouches, or diverticula, in the colon wall. This condition is common, especially in older adults, and often discovered incidentally during a colonoscopy.
Implications
For most people, diverticulosis is asymptomatic and benign. However, it can lead to complications like diverticulitis (inflammation of the diverticula) or bleeding. The risk of these complications varies based on factors such as the number and size of diverticula.
Next Steps
Patients diagnosed with diverticulosis are generally advised to follow a high-fiber diet to prevent constipation and reduce the risk of diverticulitis. Regular follow-up colonoscopies may be recommended to monitor the condition.
Inflammation or Ulcers: Indicators of Underlying Conditions
Overview
Inflammation or ulcers in the colon can indicate various conditions, including inflammatory bowel disease (IBD) like Ulcerative Colitis or Crohn's Disease, infections, or ischemic colitis.
Implications
These findings can lead to symptoms such as abdominal pain, diarrhea, and rectal bleeding. Identifying the underlying cause is crucial since the management strategies for these conditions vary significantly.
Next Steps
Further evaluation often involves biopsy during the colonoscopy to examine the tissue's histology. This can help distinguish between different types of IBD, infections, or other causes of inflammation. Treatment may include medications like anti-inflammatory drugs, immune system suppressors, or antibiotics, depending on the diagnosis.
2. Potential Follow-Up Procedures
Biopsy: A Closer Look at Cellular Insights
The Role of Biopsy in Colonoscopy Findings
A biopsy, the removal and detailed examination of tissue from the body, becomes a vital step when polyps or other suspicious areas are identified during a colonoscopy. This procedure is instrumental in determining the presence of cancerous cells or other pathologies such as inflammatory bowel disease (IBD).
The Biopsy Process
Performed during the colonoscopy, a biopsy involves snipping small tissue samples from the colon's lining using specialized instruments threaded through the colonoscope. This process is generally painless, thanks to the sedation administered during the colonoscopy.
Histological Analysis: Deciphering the Details
Once collected, the tissue samples are sent to a pathology lab where they undergo histological analysis. Pathologists examine the samples under a microscope to identify cellular abnormalities indicative of conditions like colorectal cancer, precancerous changes, or benign findings such as hyperplastic polyps.
Implications of Biopsy Results
The outcomes of a biopsy can dictate the course of action:
Benign Polyps: May require no immediate treatment but could influence surveillance intervals.
Precancerous Polyps (Adenomas): Necessitate removal and possibly more frequent surveillance.
Cancerous Cells: Lead to further diagnostic tests and the formulation of a treatment plan which may include surgery, chemotherapy, or radiation therapy.
Inflammatory or Non-cancerous Conditions: Could lead to specific medical treatments or lifestyle modifications.
Repeat Colonoscopy: Monitoring for Future Health
When is a Repeat Colonoscopy Recommended?
The necessity for a repeat colonoscopy hinges on several factors:
Polyp Characteristics: The size, number, and type of polyps removed play a significant role. Larger or more numerous polyps, especially those with high-grade dysplasia, typically necessitate closer follow-up.
Quality of Colon Cleanliness: Inadequate bowel prep may obscure the colon's view, requiring a repeat procedure to ensure no abnormalities were missed.
Family History: A history of colorectal cancer in close relatives can shorten the recommended interval between screenings.
Findings of the Initial Colonoscopy: Discovery of advanced adenomas or cancerous lesions significantly alters follow-up recommendations.
Timing of Follow-Up Colonoscopies
Guidelines for the timing of repeat colonoscopies vary:
For high-risk individuals: Surveillance colonoscopies may be advised as frequently as every 1-3 years.
For moderate risk: Intervals may extend to every 3-5 years.
For those with minimal risk: A 10-year interval between screenings is commonly recommended.
Preparing for a Repeat Colonoscopy
Preparation for a repeat colonoscopy mirrors that of the initial procedure, emphasizing the importance of a thorough bowel cleanse for optimal visibility. Adhering to prep instructions is crucial to avoid the need for additional repeat procedures due to poor preparation.
3. Importance of Regular Screenings
Early Detection: A Lifesaving Opportunity
Early detection through regular colonoscopy screenings is pivotal in the fight against colorectal cancer. These screenings are not merely diagnostic but preventive, as they allow for the identification and removal of precancerous polyps before they transform into cancer. The process of polyp formation to cancer development can span several years, offering a crucial window for intervention.
Impact on Survival Rates
The early detection of colorectal cancer dramatically improves survival rates. When detected at an early stage, the 5-year survival rate significantly increases, underscoring the life-saving potential of regular screenings. This early intervention not only enhances survival outcomes but can also reduce the need for aggressive treatments, such as extensive surgery or chemotherapy, that come with more advanced stages of cancer.
Personalized Screening Schedule: Tailoring to Individual Needs
Assessing Risk Factors
The frequency of colonoscopy screenings is not a one-size-fits-all recommendation. It is meticulously tailored, taking into account a variety of factors, including age, family history of colorectal cancer, the presence of genetic syndromes, personal health history, and the findings of previous screenings. This personalized approach ensures that individuals at higher risk receive more frequent monitoring, while those at lower risk are not subjected to unnecessary procedures.
Navigating the Recommendations
For average-risk individuals, screenings typically commence at age 45 to 50 and are recommended every 10 years thereafter, assuming no polyps are found. However, those with risk factors such as a family history of colorectal cancer may start earlier and undergo screenings more frequently. Following each colonoscopy, based on the findings, your doctor will advise when your next screening should be, creating a customized screening schedule that optimally balances risk with the procedure's benefits.
Understanding Your Colonoscopy Report: Demystifying the Findings
Deciphering the Report
A colonoscopy report contains detailed findings from the procedure, including descriptions of any polyps or abnormalities observed, their locations, sizes, and the actions taken (e.g., polyp removal). It also outlines recommendations for follow-up care or additional screenings. These reports, while comprehensive, can be laden with medical terminology that may be challenging to understand.
Sections of Importance
Findings: Details of observed conditions, from polyps to any signs of inflammation or disease.
Interventions: Descriptions of any procedures performed during the colonoscopy, such as biopsies or polyp removals.
Recommendations: Guidelines for future screenings or additional tests, based on the findings.
Fostering Dialogue with Your Doctor: Questions to Empower Your Health Journey
Seeking Clarity and Advice
An informed patient is an empowered patient. Engaging in open dialogue with your healthcare provider about your colonoscopy results and their implications is crucial. Questions you might consider asking include:
Polyp Details: Inquire about the size, number, and type of any polyps found. Understanding these details can provide insights into your risk level and the rationale behind your personalized screening schedule.
Diet and Lifestyle Recommendations: Ask for guidance on dietary or lifestyle adjustments that could reduce your risk of colorectal cancer or the formation of new polyps.
Risk Factor Clarification: Discuss any personal or familial risk factors that may influence the frequency of your screenings, ensuring you understand your specific situation and how best to manage it.
Conclusion: Empowered with Knowledge
With this guide to understanding your colonoscopy results, we hope to empower you with the knowledge to actively participate in your colorectal health management. Remember, interpreting your results is a step toward proactive health care, ensuring you remain one step ahead in your wellness journey.
Next
Warm regards,
Your Gutsphere Team
Request
Share
Our sincere request to you is to share the newsletter with your friends, family, and community so that they can benefit from the content. Also it will help us grow the newsletter, and eventually, as we release more content, digital tools, and more we will enable people around the world to live chronic disease free.
Subscribe
Feedback
Also, please give us feedback so that we can improve the content. And if there are any topics that you want us to cover please send us your questions and topics. Furthermore, if you try any of the things we provided information please share your experience with us.
Disclaimer
Please note that the information provided in this newsletter is for informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. If you have any concerns or questions about our health, please consult with a licensed healthcare professional. The information contained in this newsletter is not intended to diagnose, treat, cure, or prevent any disease. The publisher and authors of this newsletter assume no responsibility for any adverse effects that may result from the use of the information contained herein.